 View / Download pdf version of this article
View / Download pdf version of this article
Key management principles
- Provide comprehensive education and support to the child’s parents/caregivers
- Advise frequent use of emollients in adequate quantities
- Advise use of topical corticosteroids at the appropriate potency for the treatment of flares
- Seek specialist paediatric or dermatological advice in children with severe or persistent eczema
Emollients, topical corticosteroids and avoidance of triggers are the mainstays of treatment for children with eczema.
Under-use of topical treatment continues to be more of a concern than overuse. This highlights the importance of providing
comprehensive education to the child’s parents or caregivers and overcoming “corticosteroid phobia”.
Eczema affects approximately 20% of children in New Zealand, with disproportionally higher rates among Māori and Pacific
children.1 Over 90% of cases of eczema develop in children before the age of five years and 60% of these
cases occur in the first year of life.2 Although many children experience remission of their eczema as they
grow older, approximately 20 – 40% of those affected in childhood will continue to experience eczema as adults.1
Provide comprehensive education and support to the child’s parents and caregivers
Advise families how to avoid triggers and irritants, such as washing new clothes before use, using mild washing detergents
and using cotton fabrics as a base layer rather than wool or synthetics next to the skin.3, 4 The role of
food allergy in eczema is unclear. Food allergy is more likely to be a contributing factor in young infants with severe
generalised eczema. Parents should be advised against putting their child on a very restrictive diet as this is often
of limited benefit, and the diet can be expensive to maintain and result in nutritional deficiencies.
Warm (not hot) baths, are recommended for all children with eczema.5 These should be once
daily, lasting no longer than 10 – 15 minutes, and use wash-off emollients rather than soaps, detergents or bubble
baths.
Twice weekly diluted bleach baths can reduce staphylococcal carriage and improve the child’s symptoms:
this can be prepared with 2 mL of plain bleach (2.2% sodium hypochlorite) per litre of water. A full-sized bath with a
10 cm depth of water holds approximately 80 litres of water, and will therefore require approximately 160 mL of 2.2% bleach.
A baby’s bath holds approximately 15 litres of water and will require approximately 30 mL of 2.2% bleach. Avoid contact
between the bath water and the child’s eyes.
 A parent/caregiver information sheet on dilute bleach baths is available from:
www.starship.org.nz/media/269481/bleach_bath_handout.pdf
A parent/caregiver information sheet on dilute bleach baths is available from:
www.starship.org.nz/media/269481/bleach_bath_handout.pdf
For households that do not have a bath aqueous cream BP and emulsifying ointment BP (both subsidised) can
also be used as wash-off emollients applied before the child enters the shower.
At the end of bathing, the child should be rinsed off with fresh water and patted dry with a towel, followed by application
of emollients and topical corticosteroids.
The severity of the child’s symptoms should guide treatment
For all patients, use emollients frequently and in large quantities:3
- Apply several times a day and continue even when the child’s eczema has cleared
- Children should be prescribed 250 – 500 g of emollient per week to provide sufficient product for
moisturising, washing and bathing
For the treatment of flares, use sufficient amounts of topical corticosteroids, once or twice daily:3, 4
- Once daily application is adequate in most cases (preferably after a bath)
- The potency of the corticosteroid prescribed should be matched to the severity of the child’s eczema (Figure
1) and
the area of the body affected (Figure 2)
- Treatment for flares should be started as soon as signs and symptoms appear and be continued for approximately 48
hours after symptoms subside
 Best Practice Tip: Note on the prescription the specific area to which the cream needs to be applied as
this will be put on the dispensing label by the pharmacy to prevent confusion
Best Practice Tip: Note on the prescription the specific area to which the cream needs to be applied as
this will be put on the dispensing label by the pharmacy to prevent confusion
Parents often underutilise topical corticosteroids due to the fear of adverse effects. Clinicians can offer these points
of guidance to parents to help overcome “corticosteroid phobia”:6, 7
- Appropriate use does not result in skin atrophy
- The hyper- or hypo-pigmentation observed as the child’s eczema clears is usually caused by the eczema not the corticosteroid;
topical corticosteroids cause short-term vasoconstriction which may be mistaken as hypopigmentation
- The fingertip unit, i.e. the amount of product that will cover an adult index finger from the tip of the finger to
the distal interphalangeal joint, can be used as a guide for the amount of corticosteroid to be applied (Figure 3). One
fingertip unit is enough to treat an area of the child’s eczema equal to the surface of two adult hands held side by
side with the fingers together.
Pimecrolimus cream 1% (unsubsidised) is a calcineurin inhibitor that can be used in children aged three months or older
as a second-line treatment when topical corticosteroids are unable to be used or have been ineffective despite optimal
use.3
Antibiotics for secondary infection: Prescribing topical antibiotics, e.g. fusidic acid, for children with
small localised lesions of infected eczema is now generally not recommended due to the high rates of resistance to fusidic
acid in the community. The first-line recommended treatment regimen for children with infected eczema is an oral antibiotic:8
- Flucloxacillin 12.5 mg/kg, three times daily, for seven to ten days (maximum 500 mg/dose)
- If compliance with flucloxacillin is a problem, cephalexin 12.5 – 25 mg/kg, twice daily, for seven to ten days (maximum
500 mg/dose) may be used
Seek further advice for children with severe or persistent eczema: Referral pathways will vary according
to the local services available; contact your DHB.
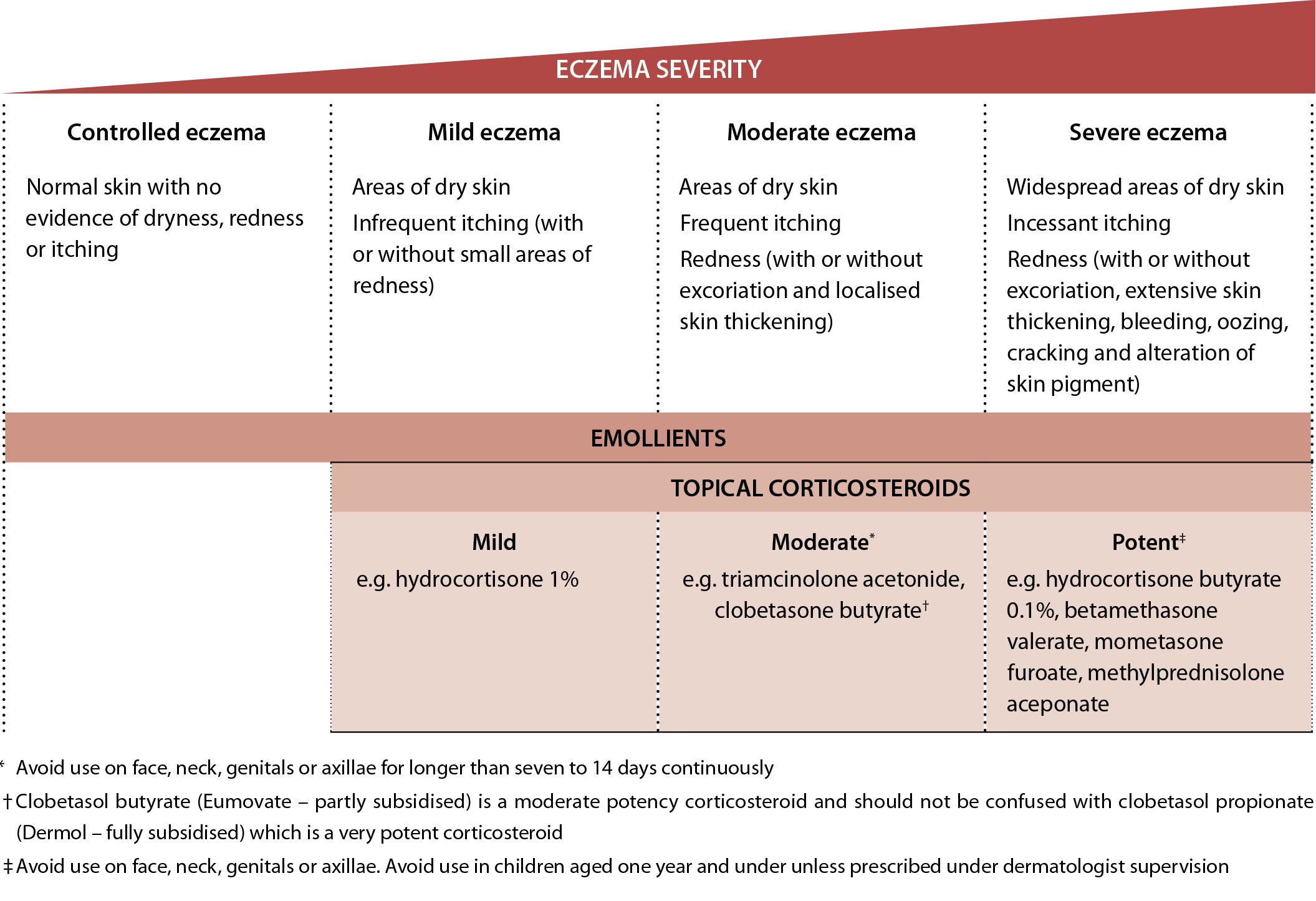 Figure 1: Eczema management algorithm (adapted from NICE, 2007).3, 9 Note that the choice of topical corticosteroid
also varies in relation to the area of body needing treatment and age of the child (see Figure 2).
Figure 1: Eczema management algorithm (adapted from NICE, 2007).3, 9 Note that the choice of topical corticosteroid
also varies in relation to the area of body needing treatment and age of the child (see Figure 2).
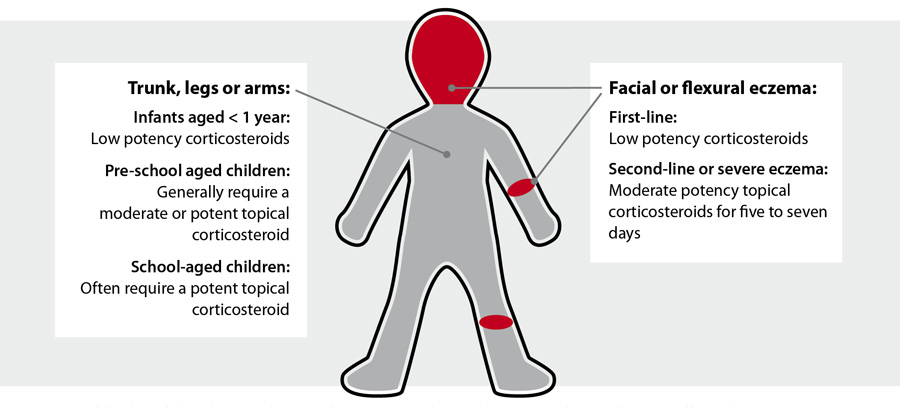 Figure 2: Useful rules of thumb to guide topical corticosteroid prescribing according to the area affected4
Figure 2: Useful rules of thumb to guide topical corticosteroid prescribing according to the area affected4
 Figure 3: Fingertip unit (Image provided by Dermnet NZ)
Figure 3: Fingertip unit (Image provided by Dermnet NZ)
 For further information, see: “Treating childhood eczema – a topical
solution for a topical problem”, BPJ 67 (Apr, 2015).
For further information, see: “Treating childhood eczema – a topical
solution for a topical problem”, BPJ 67 (Apr, 2015).
References
- Clayton T, Asher MI, Crane J, et al. Time trends, ethnicity and risk factors for eczema in New Zealand children:
ISAAC Phase Three. Asia Pac Allergy 2013;3:161–78. http://dx.doi.org/10.5415/apallergy.2013.3.3.161
- Starship Children’s Health. Child and youth eczema clinical network. Diagnosis and assessment of eczema. 2014. Available
from: www.starship.org.nz/for-health-professionals/national-child-and-youth-clinical-networks/child-and-youth-eczema-clinical-network/diagnosis-and-assessment-of-eczema/ (Accessed
Dec, 2015).
- National Institute for Health and Clinical Excellence (NICE). Atopic eczema in under 12s: diagnosis and management.
London: NICE 2007. Available from: www.nice.org.uk/guidance/cg57 (Accessed
Dec, 2015).
- Waitemata District Health Board. Eczema in children - a topical issue. 2014. Available from: http://www.saferx.co.nz//full/eczema.pdf (Accessed
Dec, 2015).
- Starship Children’s Hospital. Guidelines for the outpatient/primary care management of childhood eczema. 2014. Available
from: www.starship.org.nz/for-health-professionals/national-child-and-youth-clinical-networks/eczema/guidelines-for-the-outpatient-primary-care-managment-of-childhood-eczema/ (Accessed
Dec, 2015).
- Mooney E, Rademaker M, Dailey R, et al. Adverse effects of topical corticosteroids in paediatric eczema: Australasian
consensus statement. Australas J Dermatol 2015;56:241–51. http://dx.doi.org/10.1111/ajd.12313
- Hong E, Smith S, Fischer G. Evaluation of the atrophogenic potential of topical corticosteroids in pediatric dermatology
patients. Pediatr Dermatol 2011;28:393–6. http://dx.doi.org/10.1111/j.1525-1470.2011.01445.x
- Healthpoint Pathways. Guidelines for the assessment and management of recurrent skin infections in children > 3
months - 14 years. Available from: www.healthpointpathways.co.nz/assets/Paediatric%20Skin%20Infections/Guidelines%20for%20the%20assessment%20and%20management%20of%20recurrent%20skin%20infections%20in%20children.pdf (Accessed
Dec, 2015).
- New Zealand Formulary for Children. NZFC. 2015. Available from: www.nzfchildren.org.nz (Accessed Dec, 2015).