In this article 
View / Download
pdf version of this article
www.oneheartmanylives.co.nz
He kokonga whare ka kitea, he kokonga ngākau e kore e kitea.
‘All corners of a room may be seen, not so the recesses of the heart’. The original meaning of this
whakataukī refers to the desires of the heart. In this context the whakataukī is used to refer to the health
of the heart to go alongside the social marketing campaign for heart disease.
What is One Heart Many Lives?
The PHARMAC One Heart Many Lives programme is about the primary prevention of cardiovascular disease. It was developed
in 2003 when analysis of national data showed Māori and Pacific Island men in New Zealand, aged 35+ die 10–14
years earlier than their European counterparts. Not only do they die earlier, they do not get the right medications to
treat heart disease.
The key messages of the One Heart Many Lives programme, tell men to:
- Get your heart checked
- Know about heart disease and how to prevent it
- Inspire your fathers, brothers and friends to do the same
Activities to support the OHML programme have been focused in three key regions – Lakes, Northland and Hawke’s
Bay. “Local heroes” – Bro’ files in Northland and Tamati’s story in Hawke’s Bay – have
been used to motivate and encourage people to get their hearts checked and do something about it if the results are not
good . Community activities, advertising and media campaigns have been used to maintain awareness.
Local providers drive the OHML programme at the community level with initiatives focused around a common theme. Project
teams actively promote the consistent message “Get your heart checked” to work places and general practices
help to motivate and sustain the programme.
Outcomes of this programme include an increase in statin use. Increased CVD risk screening, smoking cessation uptake
and cost utility are other indicators being monitored.
Although One Heart Many Lives targets Māori and Pacific Island men, many Māori women have been motivated to
take action and get their hearts checked too.
One Heart Many Lives in Hawke’s Bay
Bpac has been involved in promoting OHML in the Hawke’s Bay region to general practice.
The key strategies were:
- Clinical facilitator visits to all PHOs and practices
- Providing the ability to do point-of-care testing
- Developing practice and patient information including a handbook and patient information cards
The One Heart Many Lives handbook
This handbook presented ideas on how practices could:
- Encourage Māori and Pacific men to attend general practice
- Assess their risk when they do present
- Identify manageable interventions
- Encourage them to return
- Gradually increase the amount of care they receive
Identifying at risk patients: Be prepared to seize the opportunity
Research shows that Māori and Pacific men, aged over 35 years, rarely attend primary care; any presentation then
represents a “golden opportunity”. This can be made easier by identifying these patients, setting up alerts
on PMS software and being able to offer opportunistic risk assessments. At risk patients could also be invited to attend
the practice for a free “heart check”.
Engaging patients in managing their cardiovascular risk: Get patients involved
For many men in this target group healthcare is accessed only when symptoms are experienced. As many of the factors
contributing to cardiovascular risk, such as blood pressure or cholesterol levels, usually have no symptoms, this can
make communicating the risk particularly challenging.
People are likely to respond better to learning they have an increased cardiovascular risk if:
- Increased risk is explained in an understandable and positive way
- They understand that reducing their risk is achievable and worthwhile
- They have support from whānau when they need it
Modifying risk factors: Make a start on lifestyle risk factors
It is unrealistic to expect patients to make all lifestyle changes at once. Changes are more likely to occur
if each individual prioritise lifestyle changes and sets realistic targets.
For each lifestyle change the recommended approach is to; assess a patient’s behaviour, advise about the benefits,
agree on patient centred goals, consider how your practice can assist patients attaining these goals and arrange follow-up.
What happened as a result of the OHML programme?
- Increased number of cardiovascular risk assessments
- Increased patient involvement and satisfaction with healthcare
- Increased health professional satisfaction
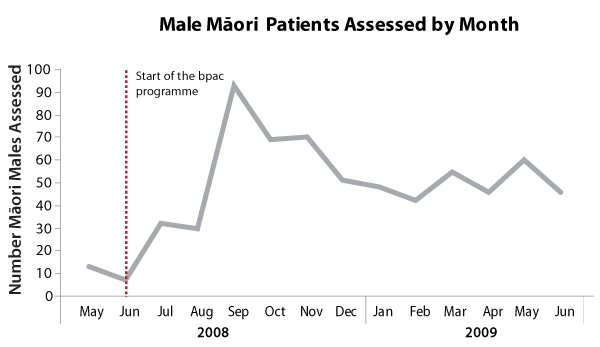
Figure 1: Number of Māori male patients assessed in all Hawke’s Bay PHOs
Increased number of cardiovascular risk assessments
After the programme started there was an increase in the number of cardiovascular risk assessments carried out
on Māori males (Figure 1). The numbers now appear to be stabilising so it is clear that continued reinforcement
is needed.
Increased patient involvement and satisfaction with healthcare
Many of the individuals who came in for a heart check had not been part of the healthcare system for years. This
process also provided opportunities for patients with other conditions to be seen by a doctor.
“One 58 year old male had a total cholesterol reading of 9.2 and a HDL reading of 0.776. This gentleman felt really
well and had not attended the practice for around two years. He was very glad that this threat to his future health had
been discovered before it was too late!”
“Another male, aged in his early 50s, had a very high BP reading – he believed that he was healthy and was
quite stunned to be told of this result. Fortunately we had the time for him to work his way through the implications
of this recording (both parents had died of heart problems in their early 60s). A free consultation with his GP was gratefully
accepted, he had not seen a doctor for around four years!”
Increased health professional satisfaction
Feedback from practices revealed that they had found the programme very positive. They felt that the programme
enabled them to make contact, and form relationships with patients who did not attend health care services, and it was
positive to see patients when they were feeling well instead of only when they are unwell.
“Because the consultations are focused on health rather than illness, I have found that patients are really interested
in health education over a wide number of topics all related to keeping healthy. This is not often the case with illness
focused consultations.”
“Quite a few of the patients who attended for CVD risk assessments had not attended the practice for around two
years, so being able to offer patients a free health assessment enabled us to make contact with these patients, and hopefully
rebuild a good relationship with them for the future.”
“All patients who had a CVD risk >15% were also given a free appointment with their GP to review the key factors
that were indicated in the review. This contact further cemented and re-established the patient’s relationship with
our practice.”
The future of One Heart Many Lives
Targeting the group of patients most at risk increases the health care provided to all others. In Hawke’s Bay,
not only did the rates of cardiovascular risk assessment increase for Māori men, they also increased for Māori
women and for the rest of the population (Figure 2).
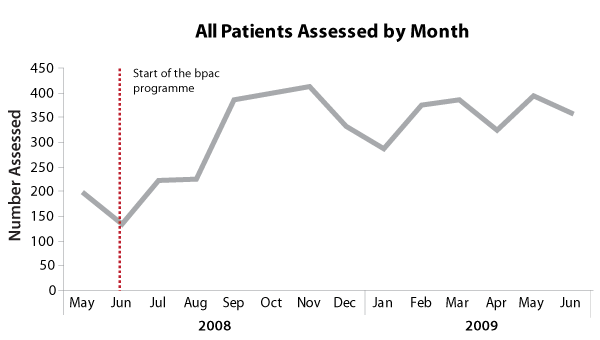
Figure 2: Total number of patient assessments in all Hawke’s Bay PHOs
How One Heart Many Lives ideas can be adapted to other areas
Obtain funding for free CVD/health checks – PHOs can apply for Services to Improve Access funding to support these
types of initiatives. For example, some PHOs have funding for targeted health checks for Māori, Pacific peoples and
those living in areas of high deprivation. Talk to your PHO about what funding is available and what services they offer.
Implement practice specific interventions to encourage the target population to attend for a free CVD/health check – target
patients can be identified using your PMS software. Various options exist once patients are identified, including inviting
patients in for a free check, or adding alerts to patient files for opportunistic assessment.
How Tu Meke First Choice PHO in the Hawke’s Bay made One Heart Many Lives work
- Obtained funding for free CVD/health checks. The PHO assisted in making the One Heart Many Lives project reach its
full potential by using Services to Increase Access funding to make the CVD/Health assessment free to the patient. The
PHO also funded follow up consultations.
- Developed practice specific interventions to encourage the target population to attend for a free CVD/health check.
One practice phoned patients in the target group to offer free assessment. Another practice sent out invitations to
those in the target group. Both reported an overwhelming response and had very few patients decline the free check.
- CVD assessments were conducted by practice nurses using point-of-care testing, to obtain non-fasting total cholesterol,
HDL and glucose. These results were used to calculate an initial estimate of CVD risk. Patients preferred to have the
result at the time of consultation and outcomes could be discussed immediately or referred to the GP.
For more information contact:
Karen Jacobs – National Programme Manager, One Heart Many Lives.
[email protected]
Phone: 04 460 4990