View / Download pdf
version of this sample report
Encouraging the appropriate use of oxycodone has been a key focus for bpacnz over the past five years. Despite a recent decrease in the number
of patients receiving oxycodone in New Zealand, there is still a large number of patients who are prescribed it each year. General practitioners are
encouraged to continue to critically review the conditions for, and appropriateness of, oxycodone prescribing in their patient population.
Key messages:1,2
- Oxycodone is a strong opioid analgesic that should be used as a second-line treatment for patients who are not able to tolerate morphine as
it does not provide more effective pain relief than morphine, is more expensive, and is associated with increasing levels of misuse.
- Oxycodone is approximately twice as potent as morphine and 7.5 – 20 times more potent than codeine, i.e.10 mg of oxycodone
is equivalent to 15 – 20 mg of morphine and 75 – 200 mg of codeine
- Oxycodone may have higher addictive potential than morphine
Oxycodone is second-line to morphine
Ideally, oxycodone should only be used in patients who do not tolerate morphine. However, in the last 12 months 86% of
New Zealand patients dispensed oxycodone in the community did not have a prior prescription for morphine. The
majority of these prescriptions (75%) were initiated in secondary care. General practitioners are well-placed
to review any indications for oxycodone prescribing, even if it has been initiated in secondary care, due
to their knowledge of a patient’s clinical history and psychosocial background.
Sample Practice Data
Between October, 2014 – September, 2015
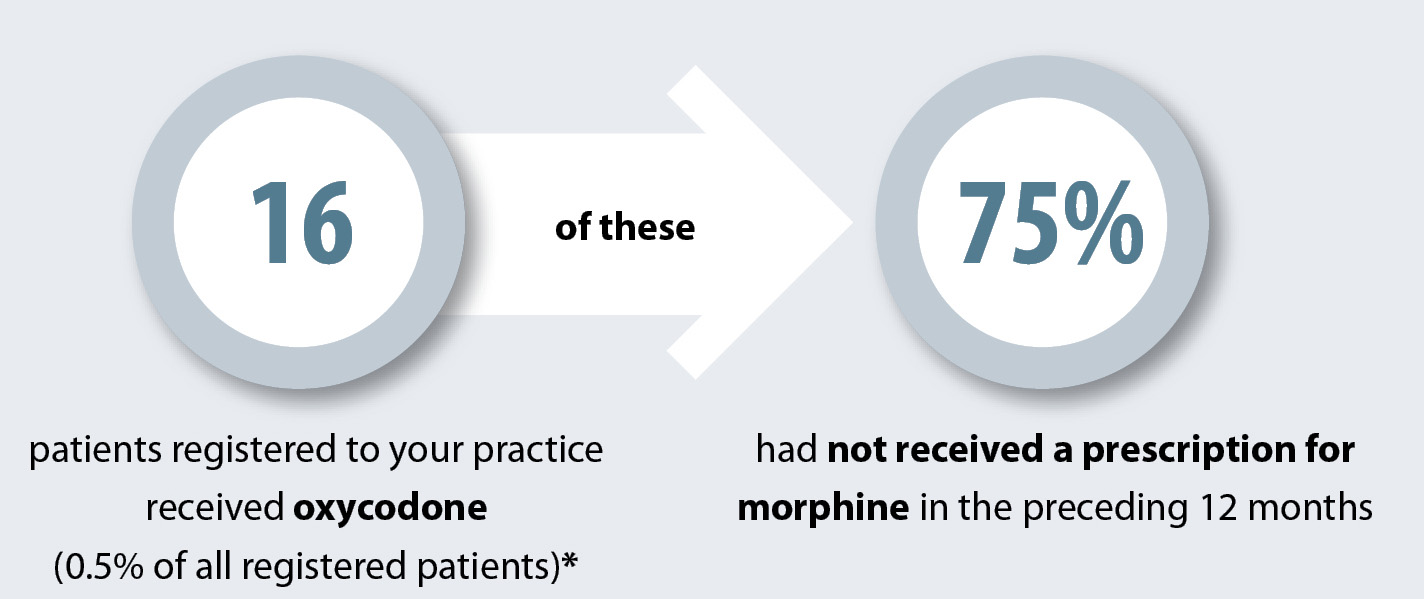
* These prescriptions may have been written by someone at your practice or by other health practitioners
Indications3
Although there are exceptions to every rule, in the majority of cases of non-cancer pain, oxycodone should only be prescribed if the patient:
- Is intolerant or allergic to morphine and;
- Has moderate to severe pain and;
- There has been an adequate trial of other treatments which have failed to control the pain
National Trends
Overall the use of oxycodone has decreased. At its peak in 2012, 13,986 patients in a three month period received an
oxycodone dispensing compared to 10,679 patients in a three month period during 2015.
The use of oxycodone varies across the country. The map on the right shows the number of patients per 1000 population in each DHB
who had an oxycodone prescription dispensed between October, 2014 and September, 2015.

Some DHBs are running safe opioid prescribing programmes, for example, the Capital & Coast DHB Integrated
Care Collaborative Programme ( ICC); this has seen a reduction in the prescribing of oxycodone through the use of prescribing
guidelines, education and audits. Contact your DHB for information on any local initiatives.
 See the audit “Oxycodone for non-cancer pain” for further information on identifying and managing patients
who have been dispensed oxycodone3
See the audit “Oxycodone for non-cancer pain” for further information on identifying and managing patients
who have been dispensed oxycodone3
- “Oxycodone: how did we get here and how do we fix it?”,
BPJ 62 (Jul, 2014). Available at www.bpac.org.nz (Accessed Feb, 2016).
- “A disaster in the making”: it’s time to take action against
misuse of oxycodone”, BPJ 61 (Jun, 2014). Available at www.bpac.org.nz (Accessed Feb, 2016).
- “Oxycodone for non-cancer pain’”. Best Practice Audit. Available
at www.bpac.org.nz (Accessed Feb, 2016).