Published: 8th December 2023
Key practice points:
- Accelerated silicosis is a progressive respiratory disease (pneumoconiosis) caused by exposure to respirable crystalline silica (RCS) when cutting artificial (engineered) stone. Dry cutting artificial stone produces very high concentrations of ultrafine silica dust that is deposited in the lungs, causing inflammation and fibrosis.
- Accelerated silicosis usually develops within ten years of first silica exposure; however, symptoms may be reported earlier following higher intensity or greater cumulative duration of exposure
- Accelerated silicosis is a relatively new disease; the first case in Australia was reported in 2015. In contrast, the more familiar chronic form of silicosis, which is associated with mining and develops over 10 – 30 years, has been recognised since ancient times.
- The prevalence of accelerated silicosis is rising in Australia. Data on the number of cases in New Zealand is still emerging but based on the estimated number of artificial stone workers, we are likely facing a problem of similar proportions.
- People can be exposed to silica dust from artificial stone for many years before they develop symptoms; however, in that time, pulmonary fibrosis and emphysema are progressing
- When symptoms do develop (e.g. mild dyspnoea with exercise, dry cough) it is generally late in the disease process and the person can rapidly advance to progressive massive fibrosis, which is characterised by scarring of lung tissue and a reduction in respiratory function. Symptoms of advanced disease include severe dyspnoea, chronic productive cough, and eventually, respiratory failure (which may require lung transplant).
- In 2020, the Accelerated Silicosis Assessment Pathway was established by the Ministry of Health, WorkSafe and the Accident Compensation Corporation (ACC), with the intent of facilitating early diagnosis in highly exposed individuals, and subsequent medical support and compensation cover:
- People who work with artificial stone are being encouraged by WorkSafe to present to their primary care clinician for an initial assessment and to lodge an ACC claim. Follow-up assessment, symptom management and long-term monitoring will be provided by ACC and respiratory physicians.
- As of September, 2023, a total of 190 claims had been lodged with the Accelerated Silicosis Assessment Pathway
- For those with early stage accelerated silicosis, disease progression may be slowed, and the risk of complications reduced, by limiting further silica dust exposure, smoking cessation (if applicable) and staying up to date with their immunisations; however, there are no effective curative treatments for silicosis and management is symptomatic and supportive
- Accelerated silicosis is preventable. Primary care clinicians should be aware of workplace safety recommendations so they can be discussed with patients, e.g. “wet working” of engineered stone with local exhaust ventilation (LEV) to minimise exposure, along with appropriate personal protective equipment (PPE) and a fit-tested well-maintained respirator to reduce any residual risk and ensure a safe work environment.
- All hazardous substance exposures, including occupational exposure to RCS, should be notified to the Hazardous Substances Surveillance System (HSSS); this can be done using the Hazardous Substances Disease and Injury Reporting Tool (HSDIRT) accessed via your practice management system, or by contacting your local public health unit directly. The local Medical Officer of Health will then notify WorkSafe if an injury has occurred.
Silica is a major component of most rocks and makes up more than half the earth’s crust.1 Mechanical processing of rock or sand releases silica dust, known as respirable crystalline silica (RCS), into the working environment.1 RCS particles are < 5 microns in diameter; small enough to reach the respiratory bronchioles and alveoli.1 The accumulation of these particles in the lungs causes silicosis, which is a progressive pneumoconiosis* resulting in chronic inflammation and irreversible pulmonary fibrosis.1 Historically, people who worked in mines or quarries were at highest risk of developing chronic silicosis, and accounts of negative health effects associated with silica dust can be traced back to Ancient Greece.2 The introduction of new technology in mining and other industries (e.g. sand blasting, artificial stone) is putting a larger proportion of the modern workforce at risk of developing silicosis.
There are three forms of silicosis which can be distinguished by the intensity and duration of RCS exposure, clinical and radiological findings and the rate of disease progression (Table 1):1, 2
- Acute silicosis (silicoproteinosis)
- Accelerated silicosis
- Chronic silicosis (simple, classical or nodular)
There is a fourth classification – complicated silicosis (also known as progressive massive fibrosis), that can either be considered a distinct disease form or a progression of accelerated or chronic silicosis.1, 2 Progressive massive fibrosis (PMF) is characterised by significantly reduced respiratory function and an increase in morbidity and mortality.1
*A group of interstitial lung diseases that result from the inhalation of dust or fibres.3 Other examples include asbestosis, coal miner’s lung, talcosis.
Pathogenesis of silicosis
The pathophysiology of silicosis is complicated and not all aspects are fully understood.1 In chronic silicosis, RCS reaches the respiratory bronchioles and alveoli, where alveolar macrophages attempt to remove it, however, due to toxicity, their phagocytic ability is reduced with prolonged or intense silica exposure.1 RCS also activates the NRLP3 inflammasome (also known as NALP3), releasing interleukin-10, transforming growth factor-β and cytotoxic T-lymphocyte antigen 4, resulting in activation of local fibroblasts.2 Initially, the fibrosis is noted as small round opacities 3 – 6 mm in diameter, visible on X-ray in the upper lobes.1, 2 In PMF, the nodule agglomerates can be larger than 10 mm.1
Acute silicosis is associated with severe alveolar inflammation, and alveolar proteinosis.1 Extremely high concentrations of RCS stimulates type II pneumocytes to oversecrete pulmonary surfactant and other proteinaceous material into the alveoli.2 The resulting local inflammation and pulmonary oedema does not resolve and is often fatal, sometimes within a few months of exposure.2, 4
The pathophysiology of accelerated silicosis is less well defined and likely involves a combination of both chronic and acute silicotic processes; evidence of nodules, fibrosis and alveolar proteinosis have been identified in the pathological findings of people who have worked with artificial stone.1
Table 1. An overview of the different forms of silicosis.1, 2, 5–7
| Disease category |
Features |
Acute silicosis
(silicoproteinosis) |
- Rare
- Results from extremely high intensity RCS exposure, e.g. abrasive sandblasting
- Can develop rapidly, e.g. weeks to five years after a period of high intensity exposure
- Alveolar inflammation and proteinosis
|
Accelerated silicosis |
- Associated with artificial stone benchtop fabrication
- Develops within three to ten years of initial RCS exposure (but often earlier)
- Can rapidly progress to progressive massive fibrosis and respiratory failure
|
Chronic silicosis
(simple, classical or nodular) |
- Historically associated with mining, e.g. coal, gold
- Develops gradually over 10 to 30 years
- Lower intensity RCS exposure
- Generally asymptomatic (mild dyspnoea on exertion, cough and excessive sputum production may be present as disease progresses)
- Pulmonary nodules < 10 mm in the upper lobes of the lungs may be seen as round opacities on chest X-ray
|
Complicated silicosis
(progressive massive fibrosis) |
- Significant pulmonary fibrosis
- Progression from accelerated and chronic silicosis (even if there is no ongoing exposure to RCS)
- Pulmonary nodules > 10 mm in the upper lobes of the lungs
- Eggshell calcification in the hila (rare)
- Advanced disease can result in respiratory failure and requires lung transplantation
|
RCS = respirable crystalline silica
Accelerated silicosis is a relatively new occupational disease; the first Australian case was reported in 2015.8 The global emergence of accelerated silicosis is closely related to the increasing popularity of artificial stone, e.g. in benchtop manufacture.1 Artificial stone, also known as engineered, manufactured or reconstituted stone, is comprised of silica and various modifiers (e.g. pigments or metals) bound in resin.2 The proportion of silica in artificial stone is typically up to 90%; significantly higher than most natural products, such as marble and granite, that contain approximately 4 – 30% silica.9
In the benchtop manufacturing industry, “jumbo-sized” slabs of artificial stone are fabricated into benchtops for kitchens, bathrooms and laundries either in purpose-built factories or on-site during assembly. Fabrication by dry cutting and polishing with power tools releases large quantities of ultrafine dust into the occupational environment.1 The concentration of RCS in artificial stone dust can be greater than 80%.9 Cristobalite, another form of crystalline silica known to be carcinogenic, and metal ions, e.g. titanium, iron and nickel, may also be present and could contribute to the disease process.1, 10, 11 Dust control measures, e.g. “wet working” (spraying water to reduce dust at the source), or wearing adequate respiratory protective equipment, minimise RCS exposure but are not consistently implemented or followed.12
Increasing numbers of people who work in this industry are being exposed to harmful levels of silica, and developing accelerated silicosis.13, 14 It is characterised by rapid disease progression, usually within three to ten years of first silica exposure.5 There are currently no data or methods to quantify the amount of RCS exposure that will result in disease; however, disease progression is heavily influenced by the intensity and duration of exposure, i.e. higher intensity RCS exposure is associated with earlier symptom development.1–3 The effects of RCS are also cumulative.11 In practice, a person with a long occupational history of RCS exposure is at higher risk of developing accelerated silicosis compared to someone who has recently started the same occupation. The shorter latency period of accelerated silicosis compared to chronic silicosis means that advanced disease is being diagnosed in younger people, e.g. aged under 45 years.15
The prevalence of accelerated silicosis in New Zealand and Australia
The prevalence of accelerated silicosis in New Zealand is not currently known, but the extent of the problem in Australia is starting to become apparent following the introduction of an industry-wide screening programme in Queensland in 2018. As of June 2022, health screening has been conducted on 1,053 people who worked with artificial stone in Queensland; 204 people were diagnosed with silicosis (19%) and 36 were diagnosed with progressive massive fibrosis (3%).16 Non-silicosis respiratory conditions were identified in 13 people.16 Other state-based screening programmes report a local prevalence of silicosis in artificial stone workers of 13% in New South Wales and 25% in Victoria.17, 18 It is likely that workplace practices and RCS exposure in the New Zealand construction industry over the last decade have been similar to those in Australia,19 meaning that the rates of accelerated silicosis will be comparable. In 2020, it was estimated that more than 500 people work with artificial stone in New Zealand.5
Other occupational activities associated with silica exposure
People who work in general construction, mining or quarrying and the stone masonry industries are also at
risk of RCS inhalation and therefore silicosis.19 Work tasks or duties that may expose people to high levels of RCS include:1
- Concrete handling, cutting, grinding or drilling
- Abrasive sand blasting, e.g. construction, automotive and textile manufacturing
- Roading or tunnelling
- Demolition, e.g. crushing or moving rock
- Excavation and earthmoving
- Cement, brick or tile manufacture
- Hydraulic fracking for oil or gas
- Pottery and ceramics
- Jewellery and ornamental stone manufacture or repairs
People with an indirect involvement in the above activities, e.g. maintenance workers, cleaners or salespeople,
may still be at risk of increased RCS exposure.3 Family members of workers carrying out high-risk activities may
be regularly exposed to RCS if clothing or equipment contaminated with RCS is not cleaned or removed before leaving the workplace.
Risk factors for developing accelerated silicosis
-
Smoking significantly increases the risk of developing accelerated silicosis, and severity (including death), in people exposed to RCS; the exact magnitude of the effect is unknown.11, 20 Smoking may potentiate the negative pulmonary effects of RCS in the same way it causes/exacerbates other respiratory conditions. Smoking cessation is strongly recommended for people who have been diagnosed with accelerated silicosis to preserve pulmonary function (see: “Management if accelerated silicosis is identified”).21
- Dry processing (also known as dry cutting), i.e. using power tools without a water source, to fabricate artificial stone releases large quantities of RCS into the occupational environment, often exceeding the workplace exposure standard (which is now 0.025 mg/m3 in New Zealand).1, 11, 22 A 2023 study involving 544 people who worked in the Australian stone benchtop industry found that 70% had been exposed to dry processing for at least 10% of their time at work.11 WorkSafe New Zealand recommends the use of on-tool water suppression to reduce silica dust (see: “Reducing silica dust exposure in the stone benchtop industry”).23
- Communication issues, e.g. language barriers for migrant workers, may limit understanding and use of safety precautions.11 It is, however, the employer’s responsibility to ensure health and safety information is clearly understood.24
Accelerated silicosis presentation
WorkSafe is encouraging people who work with artificial stone to contact their primary care clinic to arrange an assessment (see: “Accelerated Silicosis Assessment Pathway”); others may present of their own accord, with concerns about their potential risk.
Most people will be asymptomatic on presentation,5 however, symptoms should not be relied upon as a marker of disease; a relevant occupational history is the key factor in risk management.
Initial symptoms include mild dyspnoea with exercise and dry cough.5 This can progress to severe dyspnoea and a persistent productive cough in advanced disease.5 Non-respiratory symptoms, including fatigue, sleep disturbances and weight loss, may also be reported by patients with advanced disease.2, 5
Chronic complications associated with silica exposure
Respiratory failure is a well-recognised sequalae of complicated silicosis, but RCS is also considered carcinogenic in humans and increases the risk of lung and renal cancer.2 The inflammasome activation caused by RCS exposure is associated with the development of autoimmune disease (e.g. rheumatoid arthritis, scleroderma, other connective tissue disorders), and higher levels of autoantibodies have been reported in people who have been exposed to silica dust but do not have autoimmune disease, compared to the general population.2, 25 Clinicians should have a lower threshold for considering these conditions in patients with a history of occupational RCS exposure:1, 2
- Other pulmonary conditions – chronic obstructive pulmonary disease, pulmonary fibrosis, sarcoidosis, lung cancer, lymphadenopathy
- Autoimmune conditions – rheumatoid arthritis, systemic lupus erythematosus, scleroderma (Erasmus syndrome)
- Renal conditions – chronic kidney disease (including glomerulonephritis), renal cancer
- Mycobacterial disease – tuberculosis
In New Zealand, most cases of accelerated silicosis are diagnosed through the Accelerated Silicosis Assessment Pathway.5
The diagnosis of accelerated silicosis is warranted with:1
- A relevant occupational history of RCS exposure, i.e. working with artificial stone;
- Characteristic imaging findings on chest X-ray and/or high-resolution computed tomography (CT) scan; and
- Exclusion of other potential causes, such as sarcoidosis, pneumonitis and lung cancer
Typical radiological findings are graded according to the International Labour Organization (ILO) classification and include round opacities that vary in size depending on disease stage.2, 7 Symptomatic patients will likely have medium (3 - 10 mm) to large (> 10 mm) round opacities, the latter being suggestive of PMF.1, 2 Diffuse reticulonodular fibrosis, emphysema, pleural thickening, hilar enlargement or eggshell calcification may also be present.2, 26
High-resolution CT scan is favoured over X-ray for chest imaging
Interpreting the radiological results can be difficult as many features detected in people with accelerated silicosis are similar to other major lung conditions, e.g. sarcoidosis, tuberculosis and lung cancer.1 Chest X-ray has a low sensitivity in early disease; in some cases it may even appear normal.1 For example, in a 2019 study in Australia involving 78 stonemasons diagnosed with either accelerated or chronic silicosis, a normal chest X-ray (i.e. ILO grade 0) was reported in 43% of cases with an ILO classification available.13 Given the need for more sensitive testing in this context, The Royal Australian and New Zealand College of Radiologists strongly recommends using high-resolution CT scan as part of the clinical assessment of artificial stone workers.27
Accelerated Silicosis Assessment Pathway
In 2020, in response to increasing rates of accelerated silicosis in artificial stone workers overseas,
the Ministry of Health, WorkSafe and ACC established the Accelerated Silicosis Assessment Pathway (Figure 1).5 The pathway is distinct from the already established chronic silicosis pathway.5 People whose current occupation may put them at risk of accelerated silicosis, i.e. fabrication of artificial stone, are being identified by WorkSafe and encouraged to contact their primary care clinic to arrange an initial health assessment.5 This group is estimated to include over 500 people, however, anyone with an occupational history involving fabrication of artificial stone should receive an initial assessment, even if they no longer work in that industry.5 As of September, 2023, 190 claims have been lodged with the Accelerated Silicosis Assessment Pathway.28
This pathway is also used to determine if the person is eligible for ACC cover. To qualify for cover, at least some of the silica exposure must have occurred in New
Zealand (or overseas, if working for a New Zealand-based employer).5 People who were exposed to silica dust overseas but are eligible for funded public healthcare in
New Zealand should be referred to a respiratory physician for assessment.5
The updated guidance and full pathway is available on the Te Whatu Ora website (https://www.tewhatuora.govt.nz/for-the-health-sector/health-sector-guidance/diseases-and-conditions/accelerated-silicosis/accelerated-silicosis-assessment-pathway/) and is also outlined on regional Health Pathways websites (search for “silica exposure”).

ACC = Accident Compensation Corporation; CT = computed tomography
Figure 1. A summary of the Accelerated Silicosis Assessment Pathway.5
Initial health assessment for the Accelerated Silicosis Assessment Pathway
The purpose of the initial assessment with a primary care clinician is to confirm that the patient meets the exposure threshold before lodging a claim with ACC, i.e. an occupational history of at least six months of silica dust exposure in the last ten years.5 Patients should be advised that a co-payment may be required as ACC will only cover some of the costs for the initial assessment.5 A telehealth assessment may be appropriate in some situations and is permitted by ACC.5
Taking a full occupational history is essential; many people in the early stages of accelerated silicosis will be asymptomatic on presentation but further investigations will reveal evidence of disease, e.g. pulmonary nodules visible on high-resolution CT scan.11 Initial discussions with the patient should focus on:5
- Past and current silica exposure – overall period of employment in role, average duration of exposure, e.g. time spent cutting, grinding, polishing, and periods working in the vicinity of others who were working with artificial stone, specific stone products being processed
- Safety measures (see: “Reducing silica dust exposure in the stone benchtop industry”) – what measures were in place to minimise exposure and were these followed, e.g. ”wet working”, automatic machinery? Was there adequate extract ventilation on the cutting machine? Was appropriate respiratory protective equipment (RPE) worn when working with or around artificial stone? How was the RPE stored and maintained? Was adequate education and training provided, e.g. health effects of RCS and how to avoid them?
- Workplace hygiene – cleaning protocols, personal hygiene before leaving work (to prevent spreading RCS to personal vehicle and home)
- Respiratory symptom history – any current symptoms, co-morbid conditions, e.g. asthma
- Smoking history
- Dermatological or rheumatological symptoms
- Any workplace health monitoring, such as spirometry or chest X-ray. If these are available, obtain consent to include these in the patient’s medical notes and ACC claim.
- Consent – for their medical information to be sent to ACC
If practical, a physical examination should be carried out; examine for cardiac, respiratory, rheumatological or dermal abnormalities.
Any immediate health concerns identified during the initial assessment should be addressed using standard management protocols, e.g. significant respiratory symptoms requiring acute respiratory referral.5 Consider any psychological concerns and refer to an appropriate support service, such as clinical psychology service or a workplace employee assistance programme (EAP; see: “Some patients diagnosed with accelerated silicosis may require psychological support”).5
- An ACC claim should then be submitted using an ACC45 form with the appropriate identifier and relevant clinical information:5
- Read code: H42z – Silica pneumoconiosis NOS; or
- SNOMED code: 805002 – Pneumoconiosis caused by silica (disorder)
- Type of claim: Work-related
- Provide details of why you think the patient meets the exposure threshold
Clinicians should phone ACC directly if a person with a clear history of RCS exposure presents at the initial assessment with mild symptoms suggestive of respiratory disease. In some situations, primary care clinicians may choose to refer patients to a respiratory specialist who can start the assessment pathway and correspond with ACC.
For ACC contact details for providers, see: https://www.acc.co.nz/contact/
Most patients can continue to work while awaiting an ACC decision
Clinical judgement should be used when determining whether people should continue to work while waiting for the results of the ACC decision. In most cases, people will be asymptomatic and may choose to continue working in their current industry, however, steps should be taken to limit further RCS exposure (see: “Reducing silica dust exposure in the stone benchtop industry”).
People who are symptomatic at the initial assessment should not return to work where further RCS exposure could occur. ACC is responsible for developing a return to work plan and communicating this to the person, their primary care clinician and the employer.5
Follow-up assessment after lodging a claim
Once an ACC claim has been lodged, ACC will contact the person and undertake an assessment to determine if the exposure threshold and eligibility criteria are met.5 ACC will then approve a 30-minute follow-up assessment with the primary care clinician. The costs of this assessment, as well as any cost relating to investigations and secondary care referrals, will be covered by ACC, even if the claim is eventually declined.5 ACC will provide guidance regarding the next steps in the clinical assessment process and any investigations that should be arranged, including:5
- Completing the Adapted Crystalline Silica Health Form – Medical Section (available on your local HealthPathways)
- Spirometry (in clinic if equipment available, or requested via secondary care)
- Baseline chest X-ray* (PA and lateral)
- High-resolution CT scan* (as per the silica exposure protocol developed by The Thoracic Society of Australia and New Zealand)
- Laboratory tests, e.g. full blood count, autoimmune screen and urinalysis
*These should be arranged through a private provider and will be authorised by ACC.5 Information to be included in the radiology requests includes the patient’s ACC number, reference to the Accelerated Silicosis Assessment Pathway, employment and silica exposure history, smoking history, other potential causes of respiratory disease, family respiratory disease history, symptoms and other investigations that have been requested.5
Further assessment may be necessary
ACC will review the results of the follow-up assessment and recommend further investigations.5 At this point, the person may be given a diagnosis of accelerated silicosis and their cover approved, or further assessment by a respiratory or occupational physician may be required.5
If a diagnosis (and decision regarding cover) is still unclear following the occupational physician assessment, or another opinion is needed, ACC will refer the person to the accelerated silicosis multidisciplinary meeting (MDM) for review.5 The MDM comprises of occupational and respiratory physicians, rheumatologists and chest radiologists. All available information will be reviewed, and a report provided to ACC to make a final decision regarding diagnosis and cover.
Management if accelerated silicosis is identified
Guidance regarding patient follow-up and any symptom management is provided by ACC and respiratory physicians as part of the Accelerated Silicosis Assessment Pathway.5 Changing roles or occupations to prevent ongoing RCS exposure is usually recommended, however, it does not always prevent disease progression.6, 21 Practical steps that may slow disease progression and reduce the risk of complications include:3, 21
- Focused education regarding limiting further RCS exposure, especially if people choose to continue working with artificial stone (see: “Reducing silica dust exposure in the stone benchtop industry”)
- Smoking cessation (if applicable) as people that smoke are at higher risk of disease progression and complications. Discuss the importance of smoking cessation regarding preservation of remaining respiratory function and the potential impact on eligibility for lung transplantation. Offer information and advice regarding nicotine replacement therapy or other smoking cessation medicines.
- Ensuring the patient is up to date with their immunisations, e.g. influenza, COVID-19 and pneumococcal vaccines, as well as regularly checking their tuberculosis immune status
Effective intervention options for patients with accelerated silicosis are limited.21 Management usually involves symptomatic and supportive interventions to protect cardiopulmonary function (e.g. inhaled bronchodilators), maintaining a healthy body weight and undergoing pulmonary rehabilitation.21 Lung transplantation may be required in patients with complicated silicosis and respiratory failure.2
Some patients diagnosed with accelerated silicosis may require psychological support.21 The reduction in quality of life, e.g. loss of physical ability to carry out normal activities, loss of career, financial concerns and the impact of potentially receiving a terminal diagnosis will likely have a significant effect on a person’s mental wellbeing and relationships.21 Refer to appropriate mental health services as necessary.
Potential treatments for accelerated silicosis are being investigated

Bronchial lavage has been investigated as a method to remove RCS and inflammatory cells from the lungs.21 One small case study (six participants with occupational exposure to artificial stone) showed radiological improvements on high-resolution CT scan after bilateral lavage.29 Further research is required to establish if these radiological improvements resulted in improved lung function or a slower disease progression. Antifibrotic medicines, e.g. nintedanib, pirfenidone, are used to treat patients with idiopathic pulmonary fibrosis and clinical trials are currently underway to assess for an antifibrotic effect in patients with accelerated silicosis.21
Management of asymptomatic patients with a history of exposure to silica dust
A “wait and see” approach involving regular primary care-led health monitoring* is appropriate for people who have been through the Accelerated Silicosis Assessment Pathway and have no evidence of disease, or people who do not meet the exposure threshold for ACC cover. This will likely involve an annual medical examination, chest X-ray and lung function assessment,8, 24 however, individual monitoring requirements for a specific patient can be discussed with a respiratory or occupational physician.
These people should also receive tailored education regarding limiting further RCS exposure, smoking cessation and staying up to date with their recommended vaccinations.
*Employers in industries that may expose workers to RCS are legally required to provide health monitoring, however, this service will often cease if the person changes jobs or leaves the industry21, 30
Best practice tip: If you are aware that a patient works with artificial stone, place a recall to check they are taking part in workplace health monitoring. Primary care clinicians may need to provide ongoing health monitoring if this is not occurring.
Reducing silica dust exposure in the stone benchtop industry
Accelerated silicosis is preventable.1 People who work in the stone benchtop industry should be reassured that their occupation can be safe, however, education about the hazards and implementation of recommended workplace safety practices to reduce RCS exposure are critical. Clinicians should be aware of recommended workplace safety practices and be prepared to initiate discussions with those who work with artificial stone.3 These include:23, 31
- Personal protective equipment (PPE) – wear appropriate protective clothing, i.e. overalls, head cover and gloves. These should be removed before leaving work.
- Respiratory protective equipment (RPE) – wear a fit-tested and well-maintained full face (preferably air fed) or half mask respirator with the approved filter cartridge. The respirator cartridge should be replaced regularly. The respirator should be stored appropriately when not in use to prevent dust contamination, i.e. do not leave it face up on the bench next to the cutting machinery.
- Personal hygiene – wash hands before eating or drinking and prior to leaving the worksite
- Local exhaust ventilation (LEV) – workplaces should install adequate ventilation at the source of the exposure, i.e. on the machine (also referred to as local extract ventilation)
- Dust suppression – workplaces should use fabricating machinery with on-tool water suppression or extraction, wet cloths to wipe down surfaces and clean up dust with an appropriate vacuum, e.g. H-class vacuum with high efficiency particulate air (HEPA) filtration
- Scheduling – workplaces should plan tasks that will result in high levels of RCS in the environment for times where fewer employees are around, e.g. breaks or outside of normal work hours
Any concerns regarding workplace safety practices should be directed to either the employer or WorkSafe.
For information to reduce dust exposure in the workplace, see: https://www.worksafe.govt.nz/topic-and-industry/dust/8-key-things-for-workers-to-know-controlling-silica-dust-in-the-workplace/
For specific advice regarding respiratory protective equipment for workers and businesses, see: https://www.worksafe.govt.nz/topic-and-industry/personal-protective-equipment-ppe/respiratory-protective-equipment/
Australia to prohibit the use of artificial stone?
Safe Work Australia (an Australian Government statutory agency) has been considering a number of options to reduce the risks to workers developing accelerated silicosis.32 After an analysis of the evidence and the economic implications, and consultation with the industry at all levels, they have released a document that recommends the prohibition of the use of artificial stone.32 Establishing a limit on the total silica content of artificial stone, e.g. 40% silica, was considered, however, it was felt that high levels of non-compliance in the stone working industry would still put workers at risk.32 Exemptions would allow licensed businesses to continue to modify and repair previously installed artificial stone.32 At this stage, it is not known whether similar restrictions will be introduced in New Zealand.

Silicosis is not a notifiable disease, however, RCS is considered to be a hazardous substance. WorkSafe must be notified of any injury that results from a workplace exposure to a hazardous substance under Section 199 of the Health and Safety at Work Act 2015.33 This can be done using the Hazardous Substances Disease and Injury Reporting Tool (HSDIRT) accessed via your practice management system, or by phoning or emailing a notification form to your local public health unit. The local Medical Officer of Health will then notify WorkSafe.
N.B. Silica is only considered hazardous in a respirable form.
For contact details for public health services, see: https://www.tewhatuora.govt.nz/our-health-system/health-sector-organisations/public-health-contacts/
Notifying cases of hazardous substance exposures using HSDIRT
By law, injuries and diseases due to hazardous substances (Hazardous Substances and New Organisms Act 1996) must be notified to the Medical Officer of Health.
The Environmental Health Intelligence Programme NZ (EHINZ), Massey University, runs a Hazardous Substances Surveillance System (HSSS) for New Zealand. This system monitors diseases, injuries and deaths from hazardous substances exposures. Primary care notifications allow identification of substances that are causing harm and can lead to public health action to prevent disease or injury.
 For further information on the HSSS, see:
www.ehinz.ac.nz/indicators/hazardous-substances/
For further information on the HSSS, see:
www.ehinz.ac.nz/indicators/hazardous-substances/
A hazardous substance is anything that can explode, catch fire, oxidise, corrode or be toxic to humans, as defined in the Hazardous Substances and New Organisms Act 1996.
N.B. This definition does not include medicines in finished dose form (and therefore over-the-counter and prescription drug overdoses), alcohol when classified as a food, chemical toxins associated with food, nor radioactive materials as these are covered by different legislation. Manufactured articles other than those including substances with explosive properties such as fireworks are also not included, e.g. batteries.
BPAC Clinical Solutions, in association with EHINZ, and funded by the Ministry of Health, has developed a Hazardous Substances Disease and Injury Reporting Tool (HSDIRT), that permits electronic reporting of all hazardous substance exposures (Figure 2).34 It is available via Medtech, Indici, MyPractice and Profile practice management systems.34
The notification tool will show three tabs for clinicians to complete: “Exposure Event”, “Assessment” and “Notifier/Patient Details” (Figure 2). Submitting the notification will send it to your local Medical Officer of Health via a secure system. To access HSDIRT, go to the bestpractice Decision Support dashboard in your practice management system (Figure 3):
- Look for “Module List”
- Expand the “Hazardous Substances & Lead Notifications” tab
- Click on “Hazardous Subs & Lead Notifications”
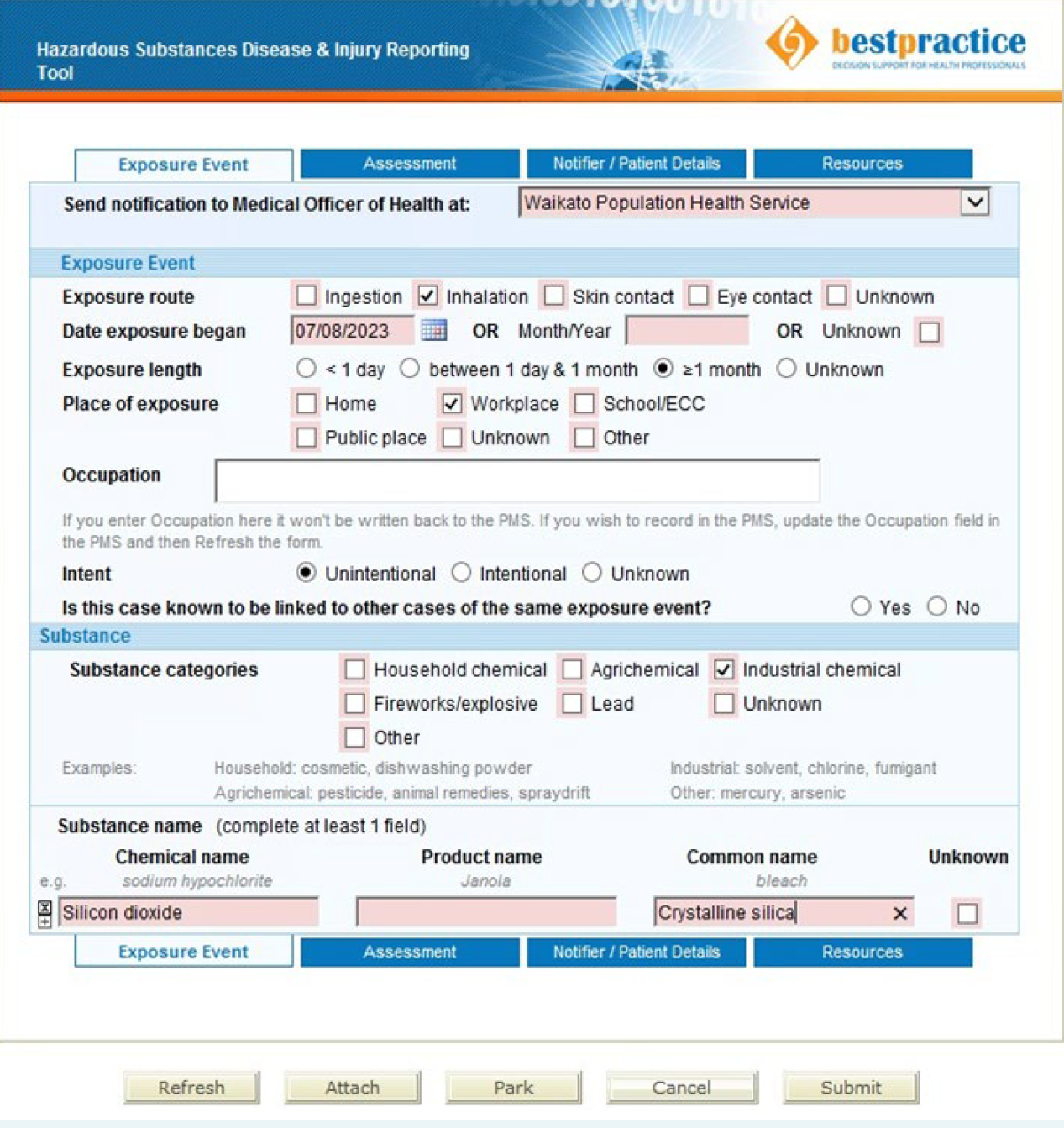
Figure 2. An example of reporting an exposure in the Hazardous Substances Disease and Injury Reporting Tool.

Figure 3. The bestpractice Decision Support dashboard.
If your practice does not have access to this tool and you want to make a notification, phone your public health unit directly.
The staff will enter the case information into a HSDIRT notification form on your behalf.34
 For a walkthrough video explaining how to access and complete HSDIRT notification forms, see: vimeo.com/359445622
For a walkthrough video explaining how to access and complete HSDIRT notification forms, see: vimeo.com/359445622
To get bestpractice Decision Support software for your practice, contact the BPAC Clinical Solutions Helpdesk:
Phone: 0800 633 236
Email: [email protected]
Website contact form: bpacsolutions.co.nz/contact/
 For further information on hazardous substances disease and injury notifications, see: bpac.org.nz/BPJ/2016/May/e-notification.aspx
For further information on hazardous substances disease and injury notifications, see: bpac.org.nz/BPJ/2016/May/e-notification.aspx





