Published: 31 January 2020
Key practice points:
- Biological medicines are complex molecules produced by living cells that target specific receptors or proteins involved
in disease progression, e.g. rheumatoid arthritis, Crohn’s disease, multiple sclerosis and some cancers;
biologicals are one of the fastest growing therapeutic classes
- A biosimilar is a comparable version of a biological medicine (the innovator) that already has regulatory approval,
i.e. the reference medicine
- The development of biosimilars reduces the overall cost to the healthcare system of biological medicines, thereby
facilitating greater patient access to treatment
- The number of funded biosimilars in New Zealand will increase as the patents on reference medicines expire. In some
cases, patients may need to be transitioned from a reference medicine to a biosimilar in order to continue
to receive the funded treatment; effective communication and provision of suitable information is essential.
- From 1 March, 2020, a rituximab biosimilar (Riximyo; Novartis*) will replace the rituximab reference medicine (MabThera;
Roche) as the funded treatment for many indications
* Riximyo is supplied by Novartis under the Sandoz brand
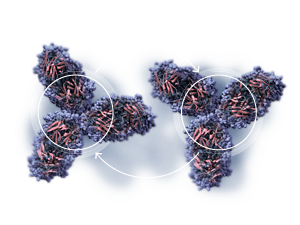
The development of biological medicines over the past 20 years has improved the treatment of conditions involving inflammatory
and immunological changes, such as rheumatoid arthritis, Crohn’s disease, multiple sclerosis and some cancers. These medicines
are typically large, complex molecules produced by genetically engineered cells that target specific receptors or proteins
involved in disease progression. Biological medicines include:
- Monoclonal antibodies* (mabs) that target a single epitope on an antigen, e.g. rituximab binds to CD20
proteins on the surface of antibody producing B cells
- Recombinant hormones†, cytokines and growth factors, e.g. insulin, erythropoietin and human growth hormone
- Fusion proteins‡, e.g. etanercept where the extracellular domain of tumour necrosis factor alpha (TNFα)
is fused to part of a human IgG protein
- Antibody-drug conjugate, e.g. trastuzumab + emtansine where the antibody is bound to a small cytotoxic molecule to
deliver the medicine to the target cells
* Created using a genetically identical population of immune cells
† Created by expressing cloned genetic material in a non-native host cell, e.g. human genes
expressed within an animal cell line
‡ Created by joining two or more genes or portions of genes that originally encoded separate proteins
Biosimilars closely resemble reference medicines but are not identical
When a manufacturer produces an innovator (reference) biological medicine, it is typically given patent protection for
ten years for the indications that the medicine has been approved for.1 Once this period has lapsed, other
companies are able to market comparable medicines to compete with the innovator medicine, after they have gained regulatory
approval. These medicines are referred to as biosimilars.
A biosimilar is comparable in all essential aspects to a biological medicine that has already been approved. Biosimilars
have robust evidence demonstrating they are not associated with any clinically meaningful difference in terms of safety
and efficacy, compared to the reference medicine (see: “Comparing the safety and efficacy of biosimilar and
reference medicines”).
Biological medicines are expensive
The average cost of developing a biological medicine has been estimated at $2.9 billion dollars (NZD) and the global
market for biologicals is predicted to be $600 billion (NZD) in 2020.2, 3 The high overall cost of biological
medicines to the health system is due to:
- The generally high price of patented biological medicines
- The increasing prevalence in ageing populations of conditions that biologicals are indicated for, e.g. cancer
- The increasing number of indications for which biological medicines are approved
- People needing to be treated for longer as life expectancy increases
Biosimilars reduce the cost of treatment
Currently, many biological medicines are not funded, or are only funded for limited indications, due to their high cost.
These medicines are therefore only accessible to people who can afford to pay the cost of treatment. Biological medicines
are likely to become more widely available as the patents for innovator biological medicines expire and competition increases,
resulting in cost reductions. Prescribing biosimilars has reduced health spending on biological medicines by 20–40% in
Europe and the United States.2 The cost of developing a biosimilar is, however, still high at $150–380 million
(NZD) per medicine and typically takes seven to eight years.3
The global uptake of biosimilars
Europe has been progressive in approving the use of biosimilar medicines. The European Medicines Agency (EMA) had approved
62 biosimilars as of December, 2019.4 Approval of biosimilars has been less rapid in the United States, with
26 biosimilar medicines being approved as of the same date.5 In Australia, 25 biosimilars had been approved
as of January, 2020, 14 of which are subsidised.6
European countries have also been proactive in encouraging the use of biosimilar medicines in clinical practice. A target
has been set in the United Kingdom for 90% of patients newly diagnosed with a condition for which a biosimilar is indicated
to be initiated on the best value biological medicine within three months.7 It is also expected that 80%
of patients being treated for more than six months with a biological should be switched to the best value medicine within
one year of that medicine being available.7 The uptake of biosimilars has been relatively rapid in many other
European countries, including Denmark and France. For example, three to four months after the patents for the TNF inhibitors
etanercept and infliximab expired in Denmark and following regulatory changes, the respective biosimilars accounted for
85–90% of the total prescribing of these biological medicines (see: “The NOR-SWITCH trial and the Danish experience:
infliximab and etanercept biosimilars“.8
Biosimilars in New Zealand
There are three biosimilar medicines currently funded in New Zealand with Special Authority Approval:9
- Zarzio (filgrastim biosimilar); recombinant human G-CSF indicated for neutropenias and for use with autologous infusions
and bone marrow transplants
- Omnitrope (somatropin biosimilar); recombinant human growth hormone indicated for growth hormone deficiency, Prader-Willi
syndrome and Turner syndrome
- Binocrit (epoetin alfa biosimilar); recombinant human erythropoietin indicated for anaemia associated with renal failure
or chemotherapy)
A rituximab biosimilar (Riximyo) will be funded from March 1, 2020 (see: “Rituximab: reference medicine
MabThera and biosimilar Riximyo”).10 There are a number of other biosimilar medicines that will be considered for funding
by PHARMAC in the near future, e.g. a trastuzumab biosimilar. As prices reduce due to increased competition among suppliers,
any biological medicine, whether a reference medicine or biosimilar, may become a newly funded brand, or have a newly
funded indication, in New Zealand.
Rituximab: reference medicine MabThera and biosimilar Riximyo

Rituximab is a chimeric murine/human monoclonal antibody that destroys antibody producing B cells by targeting CD20
proteins on their cell surface.11 MabThera (Roche) is the reference brand of rituximab and is approved in
New Zealand to treat autoimmune disorders and cancers including non-Hodgkin’s lymphoma, lymphocytic leukaemia, rheumatoid
arthritis, granulomatosis with polyangiitis and microscopic polyangiitis.28 Three patents covering the treatment
or prevention of B-cell lymphoma with MabThera expired in August, 2019, and four more patents relating to the treatment
of non-malignant autoimmune disease and rheumatoid arthritis with MabThera are expiring between 2020 and 2026.
Riximyo (Novartis*) is a rituximab biosimilar and is approved by Medsafe for the same indications as MabThera.29
* Riximyo is supplied by Novartis under the Sandoz brand
Access to rituximab will widen and a brand-change will occur:
From 1 March, 2020:10
- Riximyo will be funded for all new and existing patients requiring rituximab, except those with rheumatoid arthritis
- Riximyo will also be funded for the following new indications:
- Maintenance treatment of CD20+ low-grade or follicular B-cell non-Hodgkin’s lymphoma
- Graft versus host disease
- Antisynthetase syndrome with lung disease
- Anti-NMDA receptor encephalitis
- Severe chronic inflammatory demyelinating neuropathy
- Amending existing criteria for transplant indications to allow use for any organ
- MabThera will be funded for:
- All new and existing patients with rheumatoid arthritis
- Patients currently being treated with rituximab for all indications, other than the new indications above
From December 1, 2020:10
- Riximyo will be funded for all indications, except rheumatoid arthritis, and will be the only funded brand of rituximab
for these indications until 30 September, 2023
- MabThera will only be funded for patients with rheumatoid arthritis
Riximyo and MabThera are administered by intravenous infusion over several hours in a hospital setting
because severe infusion reactions can occur.28, 30 Premedication with an analgesic/anti-pyretic and an antihistamine
is given before each infusion.28, 30 Severe reactions generally occur within two hours of beginning the first
infusion and may include pulmonary symptoms, fever, rigors, hypotension, urticaria and occasionally tumour lysis syndrome
(with cancer treatment).28, 30
The use of Riximyo and MabThera may be associated with progressive multifocal leukoencephalopathy and patients are monitored
for the development of neurological symptoms.28, 30
Comparability between Riximyo and MabThera was demonstrated by:31
- Establishing the structural and functional characteristics of Riximyo and MabThera with comprehensive binding and
activity assays
- Non-clinical testing, including pharmacokinetics, pharmacodynamics, toxicology and experiments with a mouse xenograft
tumour model using a dose scaling design
- Assessing effector mechanisms, specifically antibody dependent cellular cytotoxicity, complement-dependent cytotoxicity
and apoptosis were assessed in whole blood assays from healthy volunteers
- Two randomised clinical trials to confirm comparability; one in patients with rheumatoid arthritis (GP13-201) and
another in patients with advanced follicular lymphoma (GP13-301)
The primary purpose of the clinical trial in patients with rheumatoid arthritis was to assess pharmacokinetics and pharmacodynamics
and establish the bioequivalence of Riximyo, MabThera and Rituxan (rituximab licensed in the United States).31 The
study enrolled 173 adult patients who had rheumatoid arthritis for at least six months and lasted for 52 weeks.31 The
primary endpoint (equivalence of clinical response) was within the standard limits for bioequivalence and therefore consistent
with biosimilarity, i.e. the ratio of the means for area under the curve (AUC) serum concentrations was 1.064 with a 90%
confidence interval of 0.968, 1.169.31
The purpose of the clinical trial in patients with follicular lymphoma was to compare the safety, efficacy, pharmacokinetics
and pharmacodynamics of Riximyo and MabThera in patients with previously untreated, advanced stage follicular lymphoma.31 Patients
(629) were given either Riximyo or MabThera in combination with cyclophosphamide, vincristine and prednisone for approximately
six months, followed by maintenance treatment with Riximyo or MabThera for two years.32 Biosimilarity was
concluded as the overall response rate was 87.1% in the Riximyo and 87.5% in the MabThera arm, with the 95% confidence
interval for the difference between the two treatments being within the pre-specified equivalence.31
Further information on the comparability of Riximyo with MabThera is available from:
www.ema.europa.eu/en/documents/assessment-report/riximyo-epar-public-assessment-report_en.pdf
In New Zealand, Medsafe applies the same regulatory standards for approving a biosimilar medicine as the European Medicines
Agency (EMA). These guidelines require the manufacturer of a biosimilar product to demonstrate that the biosimilar:1
A. Is similar to the reference medicine in terms of chemical and physical properties. This is assessed
by a range of laboratory experiments, such as antigen binding tests for antibodies. In general, there is no “gold standard”
to quantify chemical and physical similarity; the purpose of these tests is to identify any differences between the biosimilar
and the original biologic.
If the active component of a biological medicine is a protein, both the reference medicine and the biosimilar must contain
the same amino acid sequence and the same three-dimensional structure (protein folding).1 The active component
of the medicine must also be present in the same concentration and be delivered by the same route of administration.1
B. Does not have any meaningful differences from the reference medicine in terms of quality, safety or efficacy. This
is assessed by a variety of tests including pharmacodynamic and pharmacokinetic studies, as well as clinical trials of
efficacy compared to the reference biological. These tests must demonstrate that any detected differences in chemical
or physical properties do not have a meaningful impact on clinical efficacy and safety.
Microheterogeneity refers to the minor variability between reference medicines and biosimilars, e.g. small
differences in glycosylation patterns (which determine protein structure, function and stability).1 This
same degree of variability may also be present between batches of a biological medicine produced by the same company,
especially if the manufacturing process is modified during the commercial life of the medicine.1 Microheterogeneity
occurs because biological medicines are large complex molecules produced by applying proprietary technology to living
cells; they are therefore very difficult to characterise in a laboratory.11
The EMA has additional specific criteria for assessing comparability depending on the type of biological medicine under
consideration, the medicine’s mechanism of action and the safety and efficacy of the reference medicine.
Further information on Medsafe’s approval process for biosimilar medicines is available from:
www.medsafe.govt.nz/profs/RIss/Medsafe%20position%20on%20biosimilars.pdf
The EMA’s guideline on similar biological medicinal products is available from:
www.ema.europa.eu/en/documents/scientific-guideline/guideline-similar-biological-medicinal-products-rev1_en.pdf
Adverse reactions and immunogenicity
Adverse reactions associated with biological medicines may be due to administration-site reactions (mild cutaneous or
hypersensitivity reactions are common), pharmacological action or immunological reactions.12
Immunogenicity is a significant safety concern with biological medicines
The ability of a biological medicine to provoke an immune response (immunogenicity) is an important safety concern.
Immune responses to biological medicines are often limited and not severe, e.g. the transitory production of antibodies
that may decrease treatment efficacy.1 However, more serious consequences are possible including infections,
reactivation of disease, e.g. tuberculosis or cancer, and rarely systemic hypersensitivity reactions, e.g. cytokine release
syndrome (cytokine storm).12
As of 2019, there is no published study demonstrating that a biosimilar is associated with increased immunogenicity,
compared to its relevant reference medicine.13
Biosimilars and reference medicines have comparable safety profiles
The perceived concerns about biosimilars among clinicians and patients often stem from the observation that biosimilars
are “similar but not identical” to reference medicines.14, 15 Reassurance is provided by a large and accumulating
body of evidence supporting the safety and efficacy of biosimilars. A systematic review of 90 studies with more than 14,000
patients and seven different biosimilars used to treat 14 conditions found no statistically significant differences in
the rate of adverse reactions associated with the use of reference medicines.16
At an individual medicine level, comparisons of safety and efficacy between reference medicines and biosimilars often
involve switching studies, i.e. patients taking a reference medicine switching to a biosimilar (see: “The
NOR-SWITCH trial and the Danish experience: infliximab and etanercept biosimilars”). A systematic review of 63 publications involving 57
switching studies reported comparable safety and efficacy profiles between reference medicines and biosimilars in virtually
all cases, although many trials were relatively small without long-term follow-up.17 There were two exceptions
involving treatment-related adverse effects.
More
The PLANETAS extension study of 174 patients taking infliximab for the treatment
of ankylosing spondylitis, reported adverse effects during the extension phase of the study in 22% of patients on maintenance
treatment and 39% of patients who were switched to a biosimilar (CT-P13).18 Back pain and latent tuberculosis
were the adverse effects reported as being more frequent in the extension phase following the switch to the biosimilar.18 The
second exception involved 452 patients with type 1 diabetes, a subset of whom were switched to a biosimilar insulin glargine
and subsequently experienced a small, but statistically significant increase in weight of +1 kg, compared to +0.2 kg for
patients who remained on the innovator insulin; no other differences in safety or efficacy were identified.19
Once biosimilars enter the market, post-market surveillance occurs to detect unexpected responses in individuals, e.g.
rare immune reactions, or groups that may have not been studied extensively in trials, e.g. children or complex patients
with co-morbidities or polypharmacy (especially immunosuppressants).1
Extrapolation to other indications may be possible
The practice of extrapolating indications for biosimilars from reference medicines may also be a concern for some clinicians.14 Extrapolation
refers to the assumption that if there are data showing that a biosimilar is safe and effective for one indication for
which a reference medicine has approval, the biosimilar is also safe and effective for the other indications that the
reference medicine is approved for. Extrapolation only occurs if there is a substantial body of evidence demonstrating
that the biosimilar has comparable characteristics that are relevant for the specific indication1
This means that biosimilar medicines may not need the same number of clinical trials as reference medicines which must
undergo clinical trial(s) for every indication they are approved for. The practice of extrapolation results in fewer clinical
trials, thereby reducing the number of patients who need to be recruited and reducing the cost of medicine development.
The NOR-SWITCH trial and the Danish experience: infliximab and etanercept biosimilars
The NOR-SWITCH study was a double-blind, randomised trial that enrolled patients with rheumatoid arthritis, spondyloarthritis,
psoriatic arthritis, ulcerative colitis, Crohn’s disease, and chronic plaque psoriasis. The study showed over 52 weeks
that switching to the infliximab biosimilar CT-P13 (241 patients) was non-inferior to maintenance treatment with the reference
infliximab (241 patients).20 An extension trial of an additional 26 weeks, i.e. 78 weeks in total, for 380
patients was also conducted that involved patients either continuing to take CT-P13 or switching to CT-P13, if they had
been previously assigned to the reference medicine.21 In both studies it was concluded that there was no
difference in safety or efficacy between CT-P13 and the reference medicine. The primary end-point of the studies was disease
worsening, as defined by disease-specific composite measures and/or consensus in disease worsening between the investigator
and patient leading to a major change in treatment. A limitation of both studies, however, was that neither was sufficiently
powered to detect non-inferiority within individual indications.12
In Denmark, the nation-wide transition from the etanercept and infliximab reference medicines to biosimilars reportedly
did not result in any significant increase in adverse effects.8 There was also no evidence of a reduction
in treatment efficacy. In 802 patients with arthritis who had been treated with the infliximab reference medicine for
a median of 6.9 years, there were no clinically meaningful differences observed in disease activity three months after
switching to the infliximab biosimilar.22
The following factors have been identified as being critical for the successful
introduction of biosimilars into clinical practice:8, 23
- Good communication with (and between) patients and clinicians
- The provision of educational material for patients and clinicians
- Adequate time to implement changes and monitor patients for potential adverse effects
- Consistent reporting of any adverse effects
The entire healthcare team will be involved to some extent in the transition to biosimilars, e.g. prescriber
discussing the new medicine with the patient and initiating treatment, pharmacist dispensing and recording
information about the medicine (see: "Pharmacists should record the batch number...") and nurse or other clinicians monitoring patient response. In a secondary
care setting, it is recommended that each aspect of managing the introduction of a biosimilar be assigned
to one person who can act as an implementation lead.
Some clinicians may require additional reassurance to prescribe with confidence
Due to the relatively low use of biosimilars in New Zealand, some prescribers may be unfamiliar with these medicines
and require additional information in order to prescribe them confidently. A 2017 survey of 110 secondary care prescribers
(rheumatologists, oncologists, dermatologists, gastroenterologists and haematologists) showed that a minority had concerns
which included the practice of extrapolating indications, switching patients from reference medicines to biosimilars,
potential adverse effects and the amount of time it would take to explain biosimilars to patients.24 Biosimilars
are a rapidly changing area of medicine, however, and the accumulating evidence of safety and efficacy from European countries
means that knowledge and confidence about biosimilars may have increased since this survey.
Transitioning patients from reference medicines to biosimilars
Clinically any two medicines are interchangeable if they can both be prescribed for the same indication, without any
difference in clinical effect.1, 25 With biological medicines, this generally applies to changing from a
reference medicine to a biosimilar, but it is also possible to change from a biosimilar to a reference medicine or between
two biosimilars. The process of interchanging medicines may occur in two ways:1
- Switching, where the prescriber exchanges one medicine for another with the same therapeutic intent
- Substitution, where a pharmacist dispenses one medicine in preference to another without consulting the prescriber
(e.g. generic substitution); this is not approved in New Zealand for biological medicines
Therefore, biological medicine brands can be switched with mutual agreement from the prescriber and patient, but brands may not be substituted
at the pharmacy without prescriber agreement.25
Reasons to change a biological medicine brand
Prescribers may decide with the patient to switch biological medicines for reasons such as:
- To improve treatment efficacy
- To improve tolerability
- Due to issues relating to an administration device
- To reduce the cost of treatment due to funding, availability or supply issues
Effective communication is critical
If a patient is transitioned from a reference medicine to a biosimilar, communication with the patient and informed
consent needs to be carefully managed. If patients develop negative perceptions towards biosimilars they
may become anxious or concerned about their treatment, which can in turn adversely affect outcomes.15 This
is especially important for biosimilars that are self-administered, as non-adherence to treatment may
become an issue.23 Maximising
face-to-face contact with the patient during the education and consent process and providing written
and online educational material reduces the likelihood that patients will seek information from unreliable sources.
Positively framing discussions about biosimilars, while still providing balanced information about risks and adverse
effects, has been shown to increase patient willingness to switch from a reference medicine to a biosimilar, i.e. focusing
on the similarities between the two medicines.15 A New Zealand study of 96 patients currently taking a biological
medicine (35% taking rituximab) found that 67% of patients who received a positively framed message were willing to switch
to a biosimilar, compared to 46% of patients who had received a negatively framed message focusing on the differences
between the biosimilar and the reference medicine.15
Educational material for patients on biosimilars is available from:
www.fda.gov/drugs/biosimilars/patient-materials
Further information on strategies to minimise anxiety about medicine change is available from: “The nocebo
effect: what is it, why is it important and how can it be reduced?"
Prescribing and dispensing biosimilars
It is recommended that biological medicines (including biosimilars) should be prescribed by brand name, rather than
generically as is usually recommended.1 Brand name prescribing ensures that inadvertent substitution of the biological
medicine without the prescriber’s knowledge does not occur at dispensing. The use of brand names also allows for tracing
which is necessary for pharmacovigilance and quality assurance.
Pharmacists should record the batch number when dispensing biological medicines
As biosimilars become available, it is best practice for pharmacists to query any prescription for a biological that
refers to its generic rather than trade name.27 The batch number of the biological should also be recorded
at dispensing to allow tracing of the medicine, if required.12
Report suspected adverse reactions
Post-marketing surveillance of biological medicines is essential, especially when biosimilars are approved for indications
where clinical trials have not been conducted.
If a patient has a suspected adverse reaction, an adverse reaction report should be completed, including the batch
number of the biological medicine. Electronic reporting is recommended using the bestpractice adverse
reaction reporting tool in your practice management system (for more information, see:
https://bpacsolutions.co.nz/products-national-consultation-suite/).
Alternatively, an electronic form can be completed on the CARM website:
https://nzphvc.otago.ac.nz/reporting/, a report
can be made via email ([email protected]) or using the pre-printed CARM adverse reaction card.
If a patient has responded poorly to a biosimilar and the reference medicine is no longer funded for that indication,
a Named Patient Pharmaceutical Assessment application for funding may be necessary. Further information is available from:
https://pharmac.govt.nz/medicine-funding-and-supply/make-an-application/
Further information on reporting adverse effects is available from: The New Zealand Formulary (NZF):
www.nzf.org.nz/nzf_107 Medsafe:
www.medsafe.govt.nz/safety/report-a-problem.asp
and
www.medsafe.govt.nz/profs/PUArticles/June2019/The-fantastic-four-of-adverse-drug-reaction-reporting.htm





