The concept of frailty describes vulnerable people who have an increased risk of adverse outcomes, including falls,
loss of independence, worsening disability, need for residential care and death.1 This vulnerability can
be attributed to accumulated losses in physiological, psychological and/or social functions, which impairs the ability
of the person to cope with, and recover from, challenges to their health, i.e. illness, injury, surgery.1, 2 For
a person with frailty, even a small challenge, such as being prescribed a new medicine, a minor infection or a fall without
injury, can cause a dramatic and disproportionate change to their health state, e.g. from lucid to delirious, independent
to dependent, mobile to immobile.1
There is currently no consensus as to how frailty is defined clinically, however, a combination of the following parameters
may be considered as part of a diagnosis:1
- Unintentional weight loss, usually associated with a loss of muscle mass (i.e. sarcopenia)
- Weakness (grip strength)
- Slow walking speed
- Self-reported exhaustion
- Low physical activity
- Cognitive impairment
- Social isolation, depression
- Disability and chronic disease
- Clinical presentations, e.g. falls, incontinence or delirium
Often knowledge of the patient’s medical history and circumstances will guide a clinician to identify frailty without
the need for a formal assessment, e.g. if they need assistance in their daily activities or to do their grocery shopping,
or they are in long-term residential or hospital-level care, then they likely have frailty. Some of this information may
come to the clinician indirectly from family members, whānau or other caregivers who notice changes to their relative’s
health state. Patients may be reluctant or unable to share this information themselves, possibly due to fear of the consequences,
e.g. potential loss of independence, denial over their declining health, or because they are unaware, e.g. cognitive impairment.
Why is frailty important?
Frailty may be considered as part of the continuum of normal ageing toward eventual disability and death which results
from a progressive functional decline in multiple organ systems.3 Frailty manifests when the functional decline
crosses a “threshold”, meaning that the person can no longer physiologically adapt to health challenges.2 The
rate at which people reach and move through this continuum varies and cannot be defined by a specific chronological age.3 Genetics,
family history, lifestyle factors (e.g. smoking), diet and exercise all contribute to the rate at which functional decline
occurs, and may result in a discrepancy between the biological age of a person and their chronological age. Many people
remain active and resilient to health challenges as they age, while others may have increased vulnerability, e.g. due
to chronic illness or disability, and have frailty at a younger age.1
Frailty can be regarded as a “risk” state, where a person with frailty is more likely to have an adverse outcome in
response to a health challenge than a person without frailty. Often clinical guidelines will include chronological age
in their recommendations, however, in some situations it may be more appropriate to make treatment or intervention decisions
based upon the frailty status of the patient, i.e. if the outcome is likely to be affected by this state of increased
vulnerability, such as initiating a new medicine or referring for a major surgical procedure.
Frailty is associated with ageing, not defined by it
While frailty is not defined by chronological age, it becomes more common with advancing age.1 The prevalence
of frailty* among people aged ≥65 years is approximately 10%, increasing to approximately 26% in people aged ≥85 years.1 A
longitudinal study conducted in the United Kingdom estimated that 65% of people aged >90 years have frailty.4 These
estimates are consistent with data collected from the Living Standards of Older New Zealanders survey (2001)** where the
overall prevalence of frailty was 8%, lower in those aged 65 to 74 years (6%) and increased in those aged 85 to 94 years
(20%).5 Approximately 44% of people aged ≥65 years have features indicative of the early stages of frailty*.1
These data highlight the variability in the health needs of older people. It is also important to be aware that many
older people do not have frailty and are likely to be more resilient to health challenges than people with frailty, regardless
of their chronological age.
* Defined by the presence of three or more out of the following five criteria: unintentional weight loss, weakness,
slow walking speed, self-reported exhaustion, low physical activity.1 The presence of one or two of these
features indicates the early stages of frailty (also referred to as “pre-frailty”).1
** This study defined frailty as having six or more medical, physical or mental health problems, and difficulties carrying
out activities of daily living.
Females and Māori are at an increased risk for frailty
Frailty is more common among older females than older males; however, males with frailty have an increased risk of all-cause
mortality compared to females.5, 6 The underlying reasons for this difference are complex and not fully understood,
but predominantly relate to females having a longer lifespan than males.
The presence of co-morbidities, socioeconomic deprivation, smoking, and being obese (body mass index [BMI] >30) or
underweight (BMI <20) are associated with an increased prevalence of frailty.5, 7, 8 Abdominal adiposity
(as measured by waist circumference >88 cm for females or >102 cm for males) in particular is associated with an
increased risk of frailty, even in people with a healthy BMI.8
Māori are more likely to have frailty than non-Māori (11.5% versus 7.9% of people aged ≥65 years) and at a younger age,
e.g. the prevalence of frailty among Māori aged 65 to 70 years is similar to non-Māori aged 81 to 84 years.5 This
likely due to the earlier onset of chronic disease and a higher prevalence of other risk factors, e.g. smoking or obesity,
in this group. These factors may also increase the risk of frailty in people of Pacific ethnicity.
Frailty is common among people with one or more long-term condition.1, 7 Evidence from a study conducted
in the United Kingdom including over 490,000 middle aged and older adults, found that multiple sclerosis, chronic fatigue
syndrome, chronic obstructive pulmonary disease, connective tissue disease, diabetes, cerebrovascular disease, cardiovascular
disease and depression were most commonly associated with frailty.7 Adverse outcomes in relation to any co-morbidities
are increased by the presence of frailty, e.g. a small study of patients with cardiovascular disease (CVD) undergoing
percutaneous coronary interventions reported a three year mortality rate of 28% for those who had frailty compared with
6% in those who had CVD without frailty.9 The risk of all-cause mortality is substantially higher in older
adults with frailty than those without.7, 10
People with frailty have a higher risk for post-operative delirium, in-hospital mortality and mortality at one-year
following a surgical intervention compared to people without frailty.11, 12 They are also more likely to
spend longer in hospital and require further care or rehabilitation once they have been discharged.11
Falls and frailty go together
Falls are common among older people. People aged >65 years have a one in three chance of a fall each year, increasing
to a one in two chance for people aged >80 years.13, 14 A fall in an older person can significantly impact
their health and wellbeing, increasing the risk of hospitalisation, need for residential care and death.13
The relationship between frailty and falls is bidirectional; frailty is an important risk factor for falls and falls
can lead to frailty in someone who was previously healthy.13 The increased falls risk associated with frailty
may be due to:15
- Musculoskeletal changes affecting mobility, e.g. reduced muscle mass and strength
- Postural hypotension, which may be caused by decreased venous return to the heart, a consequence of reduced muscle
mass and strength, a slowed baroreflex, or medicines that lower blood pressure
- Adverse reaction to a medicine, e.g. anticholinergics, sedatives, benzodiazepines and psychotropic medicines, or a
combination of medicines with additive effects
Identifying people at risk of falling and setting in place strategies to prevent falls can help to keep older people
with frailty independent and out of hospital. Some examples of strategies to reduce falls risk are:
- Exercise interventions to improve strength, balance and co-ordination
- Recommending changes to the home environment, e.g. removing mats, improving lighting, adding hand rails
- Encouraging the use of mobility aids, e.g. walking stick or frame
- Reviewing prescriptions to identify medicines associated with a risk of falls
For further information on the causes and prevention of falls in older people, see:
www.bpac.org.nz/BPJ/2010/March/falls.aspx
To access the Stay Independent Falls Prevention Toolkit, see: www.bpac.org.nz/falls/
Identifying frailty in primary care
Clinical experience will often guide a health care professional to identify frailty,
however, if a more objective assessment
is required, the timed-up-and-go-test can be used as a quick and sensitive measurement of frailty and risk of falls.1,
13 The test records the time taken for a person to get up from a chair, walk three metres, turn around, return to
the chair and sit down. If it takes more than 12 seconds to complete the test, frailty and a high risk of falling is more
likely.13
Grip strength may also be used to assess frailty.1 This can be tested by asking the patient
to grip onto your fingers as tightly as they can, and subjectively measure their grip strength, or it can be measured
precisely with a hand-held dynamometer.
A number of other assessment tools have been developed to facilitate the identification of frailty in a clinical setting.3 These
typically involve a questionnaire-based approach, but may also include physical measurements.1, 3 However,
the clinical utility of such tools in a primary care setting is limited, often due to the time required to complete the
assessments or lack of proper validation.
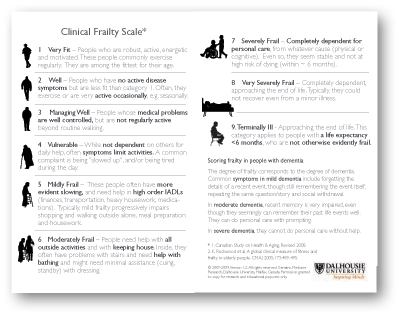 One example of a validated frailty assessment tool which may be useful in primary care is the Clinical Frailty
Scale.16 This tool identifies frailty according to a nine-point scale ranging from very fit through
to terminally ill, with stages of vulnerability, i.e. frailty, in between. The scale is based on understanding of the
individual patient’s circumstances, e.g. reduced mobility, needs assistance with activities of daily living, rather than
requiring an objective measurement of frailty, e.g. walking speed or grip strength. For patients with dementia, the severity
of dementia corresponds to the severity of frailty, even if they appear to be more physically robust.
One example of a validated frailty assessment tool which may be useful in primary care is the Clinical Frailty
Scale.16 This tool identifies frailty according to a nine-point scale ranging from very fit through
to terminally ill, with stages of vulnerability, i.e. frailty, in between. The scale is based on understanding of the
individual patient’s circumstances, e.g. reduced mobility, needs assistance with activities of daily living, rather than
requiring an objective measurement of frailty, e.g. walking speed or grip strength. For patients with dementia, the severity
of dementia corresponds to the severity of frailty, even if they appear to be more physically robust.
The Clinical Frailty Scale can be found here:
www.dal.ca/sites/gmr/our-tools/clinical-frailty-scale.html
Cognitive impairment, dementia and depression have also been shown to contribute to the reduction in
physical activity which is characteristic of frailty, and are risk factors for falls in older people.17, 18 If
cognitive impairment or dementia is suspected, a screening tool such as the six-item cognitive impairment test (6-CIT)
or the Mini Assessment of Cognition (Mini-COG) may be used. Depression can be identified in older people
using the 15 question Geriatric Depression Scale where a score of more than ten is indicative of depression.
For further information on assessing cognitive impairment in older
adults, see:
www.bpac.org.nz/BPJ/2009/September/senior.aspx
For further information on the diagnosis and management of depression in older adults, see:
www.bpac.org.nz/BPJ/2011/July/causes.aspx and www.bpac.org.nz/BPJ/2011/July/management.aspx
The cognitive function and depression screening tools can be accessed on the following websites:
The impact of frailty upon the efficacy and safety of many medicines is not known. People with frailty are almost always
excluded from clinical trials and consequently the optimal dose, therapeutic response and adverse outcomes associated
with medicines are unknown in this group. Medicines should be used carefully in people with frailty to minimise potential
harm, i.e. start at a low dose and increase slowly if required, with close monitoring for adverse reactions. Dose adjustment
may be required for medicines that were initiated in patients at a younger age or when frailty was not present. For example,
it may be appropriate to reduce the dose of antihypertensives or diabetes medicines to reduce the risk of falls and hypoglycaemia,
respectively.
For further information on de-intensifying treatments, see: “Stopping medicines in older adults” available from,
www.bpac.org.nz/2018/stopping.aspx
For information on prescribing particular medicines for older people and any recommended dose adjustments, refer to
the New Zealand Formulary: www.nzf.org.nz
Age-related declines in receptor sensitivity, renal and hepatic function, as well as changes to body composition, i.e.
increased fat mass to lean mass ratio, may mean that dose adjustments are necessary for older people with frailty.15,
19–21 For example, reduced renal clearance of medicines may increase the risk for an adverse reaction
at a standard dose. This is particularly relevant for medicines with a narrow therapeutic window that are renally excreted,
e.g. digoxin.
Estimating renal function in older people with frailty
Renal function is typically estimated by measuring serum creatinine and calculating the estimated glomerular filtration
rate (eGFR).21 However, in people with low muscle mass, i.e. older people with frailty, serum creatinine
levels may appear to be in the normal range, leading to an overestimation of eGFR.15 The Cockcroft-Gault
equation, used to calculate creatinine clearance, is an alternative method for estimating renal function and is recommended
for older adults as it accounts for bodyweight and is therefore more accurate than eGFR.15, 21 However, a
conservative interpretation of renal function, and any dose adjustments based upon this estimate, is still recommended
to minimise potential harm. For example, the Cockcroft-Gault method might overestimate renal function in people with frailty
who are also obese as the equation uses total body weight, which will be higher in these people, despite having low muscle mass.
A Cockcroft-Gault calculator can be found here:
www.nzf.org.nz/nzf/resource/Creatinine%20Clearance%20Calculator.htm
For further information on prescribing medicines for people with renal impairment, refer to the New Zealand Formulary:
www.nzf.org.nz
How to approach prescribing in older people with frailty
The World Health Organization’s guide to good prescribing provides an effective framework for prescribing medicines
to older people.19 The frailty status of the patient should be considered at each step as follows:15,
18
- Define the problem: older people with frailty may present with falls, incontinence or delirium. While
the clinician or patient may attribute these events to normal ageing, often they are the result of an adverse
reaction to a medicine. A medicine review should be carried out for older patients that present with any of these conditions.
- Specify the therapeutic objectives: the goal of treatment should be to improve quality of life through
control of symptoms or prevention of disease. For patients with limited life expectancy, the vulnerability
and increased susceptibility to adverse reactions are likely to outweigh the benefits of some medicines, e.g. aspirin,
statins, bisphosphonates or proton pump inhibitors.
- Verify the suitability of the treatment: the benefit of the medicine must be considered in relation
to any co-morbidities, potential medicine interactions and the therapeutic objectives. As frail older people
are often excluded from clinical trials, the efficacy and safety of many medicines in this group is unknown.
- Initiate treatment: adjust the dose of the medicine to account for pharmacokinetic and pharmacodynamic
changes in people with frailty, e.g. a lower dose may be required to achieve the therapeutic goal.15 Only
initiate one medicine at a time so that any changes to the patient’s condition, including any adverse reactions,
can be accurately documented and addressed.
- Give information, instructions and warnings: information should be provided to the patient and their
caregivers; warnings should include monitoring for adverse reactions, particularly as these might manifest
as reduced mobility, falls or confusion. Ensure a clear plan is also recorded in the patient’s medical notes.
- Monitor (and stop) the treatment: once the therapeutic target has been reached, the medicine can be
stopped (if appropriate, i.e. not a chronic condition requiring ongoing treatment). Only one medicine should
be stopped at a time. The dose should be reduced gradually if required and the patient monitored for any discontinuation-related
adverse effects or recurrence of symptoms.
Consider stopping medicines in older people with frailty
Older people often have multiple co-morbidities, increasing the rate of polypharmacy and the risk of frailty.19 An
Australian study of over 1500 older males, reported polypharmacy (five or more medicines) in 65% of males with frailty,
compared to 27% of males without frailty.23 For many older patients polypharmacy is necessary; however, the
increased risk of adverse reactions associated with polypharmacy (medicine-medicine or medicine-disease interactions),
and the susceptibility of people with frailty to these reactions, means medicines should be reviewed frequently to minimise
the risk of harm.19
One of the aims of reviewing a patient’s medicine regimen is to withdraw medicines which no longer provide a therapeutic
benefit, where the evidence does not support ongoing use, or where the risk of harm outweighs the benefits of continued
use. Once medicines that could be stopped have been identified, develop a plan for stopping in consultation with the patient
that is appropriate for the medicine (e.g. abruptly stopping or slowly decreasing the dose over a period of time), stop
one medicine at a time and monitor the patient for symptoms of withdrawal or recurrence of the condition being treated.15 N.B.
Some medicines need to be decreased gradually over time to reduce the risk of serious discontinuation-related adverse
effects, e.g. antidepressants, sedatives and hypnotics, opioids, antiepileptics and beta-blockers.15
For a focused discussion on de-prescribing, see: “Stopping medicines in older adults” available from,
www.bpac.org.nz/2018/stopping.aspx
There are currently no interventions known to reverse frailty, however, there are some strategies that can help slow
its onset and progression in older people.
Exercise may help prevent the progression of frailty
Exercise, particularly resistance-based exercise, improves muscle mass and function, and reduces the risk of falls.13,24 Group
exercise activities may be more effective than solitary exercise for preventing the progression of frailty, possibly due
to the added social and cognitive aspect.24
The optimal frequency, duration and intensity for exercise interventions aimed at preventing or slowing the progression
of frailty has not been determined, however, the recommended target for all older adults is 30 minutes of aerobic exercise
per day, five days a week, plus an additional two or three sessions each per week of resistance training and balance/flexibility
activities.24, 25 This target may not be suitable for all people and starting with low-intensity exercise one
or two days a week and building up to five days a week may be a more appropriate goal.
Green prescriptions can provide the patient with a support person who will encourage physical activity through
telephone calls, face to face meetings or in group settings, see: www.health.govt.nz/our-work/preventative-health-wellness/physical-activity/green-prescriptions/green-prescription-contacts
To find out which exercise groups are available in the local area, see: www.livestronger.org.nz
For an example of an exercise prescription that may be appropriate for a person with frailty, see: www.pulmonaryrehab.com.au/importance-of-exercise/exercise-prescription-table/
Nutritional interventions to prevent the progression of frailty
For older people who are underweight, increasing their daily calorie intake may help to slow or prevent the progression
of frailty.24 If the patient cannot manage this through diet alone, a nutritionally complete food supplement
(e.g. Ensure or Fortisip) may help them increase their daily calorie intake. Ensuring adequate dietary protein intake
is important for helping prevent the age-related decline in muscle mass and strength which is closely associated with
frailty.26 For older people who are obese or have increased abdominal adiposity, lifestyle interventions such
as increasing exercise and making healthy food choices should be recommended.
For further information on optimising nutrition in older people, see: www.healthed.govt.nz/system/files/resource-files/HE1145_Eating%20for%20healthy%20older%20people.pdf
Low vitamin D levels are associated with frailty
Older people with vitamin D deficiency are at an increased risk for frailty, however, the evidence supporting the success
of interventions targeting this nutritional deficiency to prevent or slow the progression of frailty is limited.27 Vitamin
D levels are usually maintained by exposure to sunlight, however, this can be difficult for people who have limited mobility,
e.g. people in residential care. Vitamin D supplementation may therefore be considered for people with frailty who have
reduced mobility and are unlikely to get adequate sun exposure.28
For further information on improving nutrition in older people, see: www.bpac.org.nz/BPJ/2011/May/elderly.aspx
For further information on vitamin D supplementation, see: www.bpac.org.nz/BPJ/2016/July/supplementation.aspx
Resources from the Goodfellow Unit which provide further information on frailty in older adults are:





