- In New Zealand, there has been an increasing rate of antibacterial resistance in Staphylococcus aureus, a frequent
causative organism in skin infections such as impetigo and infected eczema
- Research shows that this increasing resistance has occurred in association with high rates of topical antibiotic
use
- Infectious disease experts believe that there are now few clinical situations in which topical antibiotics are appropriate,
and that in the near future they may no longer be recommended at all
Clinical indications for the use of topical antibiotics are continuing to narrow, driven by increasing resistance rates
in New Zealand. Questions as to whether these medicines should be prescribed at all are now being asked. It is a rapidly
changing landscape and for the third time in as many years we are highlighting the issue of antimicrobial resistance and
updating recommendations on the appropriate use of topical antibiotics.
For further information, see: “Topical antibiotics for skin infections: when are they appropriate?”
Concerns about antimicrobial resistance (AMR) are increasing in New Zealand and worldwide.1, 2 AMR is now
considered to be one of the most significant issues in healthcare.1 Education for both prescribers
and patients to promote the responsible use of antibiotics is an important strategy to reduce AMR.
Excessive use of topical antibiotics is known to be a key driver of AMR, and is directly responsible for increasing
antibacterial resistance in S. aureus.3, 4 There have been calls to restrict the use of topical
antibiotics for some time, both in New Zealand and internationally.5 ,6 It is clear that this need is becoming
more urgent.3, 7 New Zealand research has shown significant associations between increases in the use of
topical mupirocin and fusidic acid and rapidly rising resistance rates in S. aureus (Figure
1).3, 4 Similar findings have been reported from the United Kingdom and Australia.5, 8 It
is noteworthy that topical fusidic acid is not licensed for use in the United States and rates of fusidic
acid resistance are negligible.5
There are three major reasons why resistance to topical antibiotics is important:5, 7
- Increasing resistance leads to ineffective treatment with these medicines
- There can be associations with other antimicrobial resistance, e.g. selection for fusidic acid resistant strains also
selects for methicillin resistance
- Increasing resistance to topical forms of antibiotic medicines threatens the effectiveness of oral and intravenous
formulations of the medicines, e.g. oral fusidic acid which has a role in the treatment of invasive infections, e.g.
of bones and joints
Although there is a not yet a large evidence base to support the efficacy of topical antiseptics for treating skin infections,
the consensus is that, given rising antibacterial resistance rates in New Zealand, they present a logical alternative
and should be used in place of topical antibiotics in most cases,7, 11 along with education about good skin
hygiene practices.
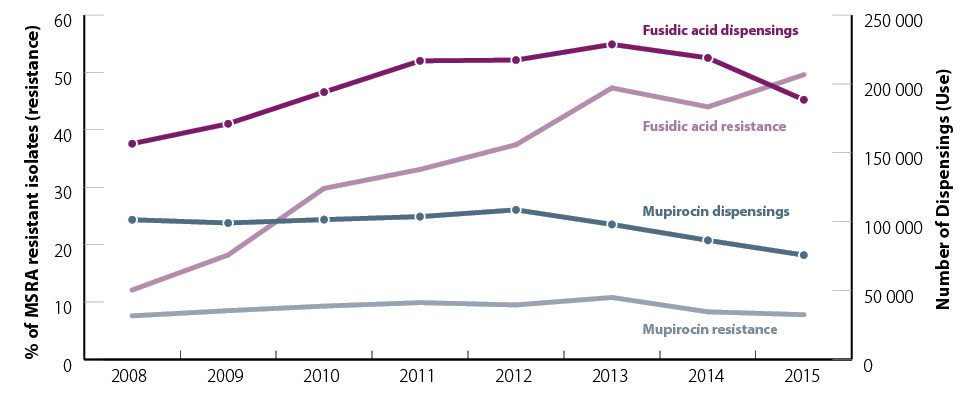
Figure 1. The annual number of community-dispensed prescriptions for mupirocin and fusidic acid from 2008
to 2015 and the percentage of methicillin resistant S. aureus (MRSA) isolates resistant to mupirocin and fusidic acid9,
10
In the one year period, from July, 2015 to June, 2016, approximately 189 000 prescriptions for topical fusidic acid
and 74 000 for topical mupirocin were dispensed in New Zealand.9 Although the number of dispensed prescriptions
for fusidic acid has decreased from a peak of approximately 220 000 in 2013, and mupirocin prescribing is also slowly
declining (Figure 1), experts believe prescribing rates remain too high. Fusidic acid was the 54th most prescribed medicine
in New Zealand between July, 2015 and June 2016, giving it a similar ranking to medicines such as topical hydrocortisone
products, lactulose and erythromycin.12
Dispensing rates for fusidic acid are highest in young children (< 5 years), in Māori and Pacific peoples and in
people living in the North Island (Figure 2).9 This reflects higher rates of skin and soft tissue infections
in these groups.3, 4 ,7
For further information on prescribing trends, see: “Prescribing of topical medicines for skin infections”
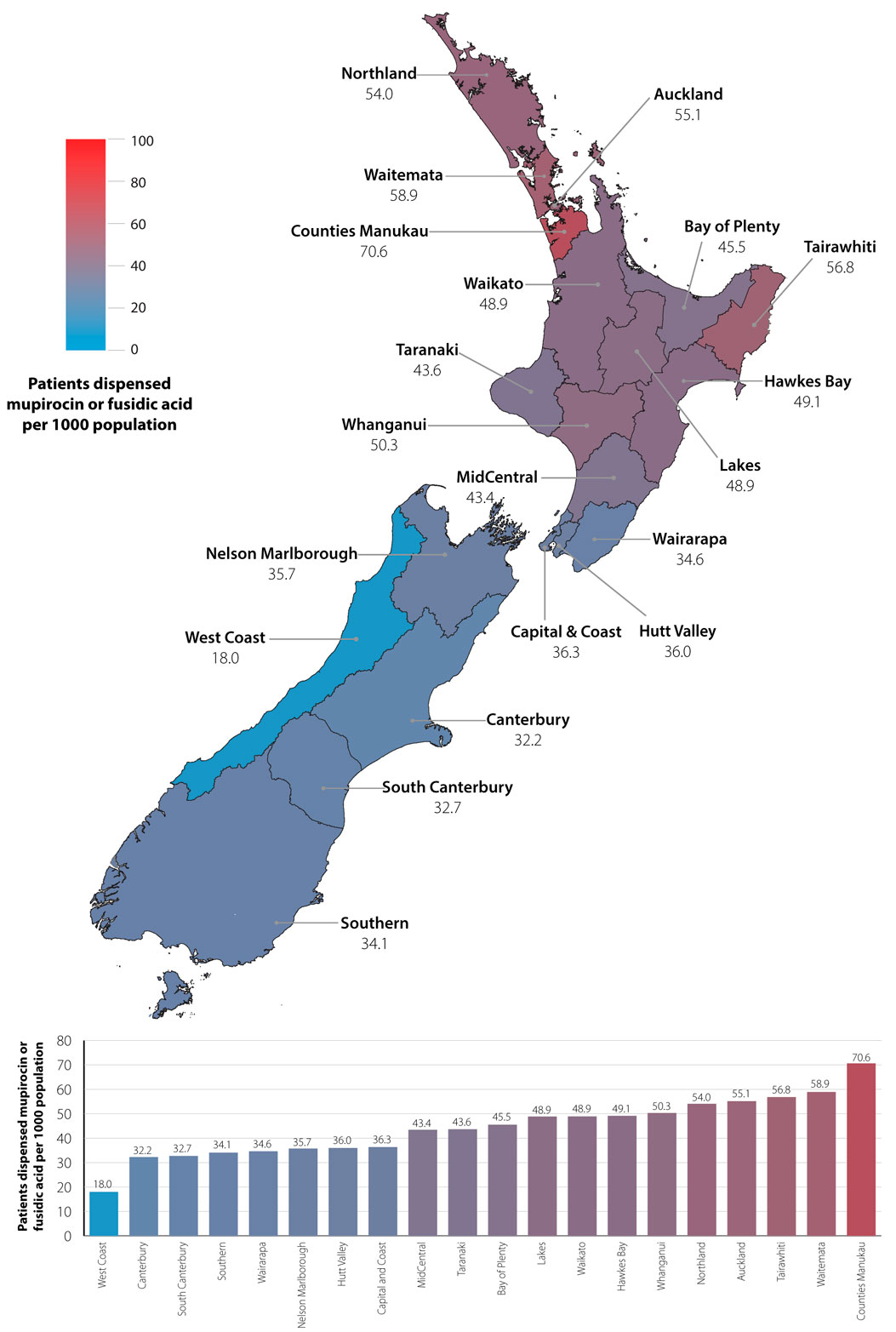
Figure 2. July, 2015 to June, 2016 dispensing rates by District Health Board for mupirocin or fusidic acid
A number of factors are likely to contribute to the inappropriate use of topical antibiotics in patients with skin infections,
including:2
- Diagnostic uncertainty – is this a bacterial infection?
- Lack of clinical knowledge – is an antibiotic indicated for this patient or not?
- Apprehension – will the patient be treated correctly or will there be a bad outcome?
- Patient expectation – my infection requires antibiotic treatment, if the clinician does not treat me, they are not
doing their job
The difficulty for prescribers is that there are often no easy solutions. Rapid diagnostic tests and biomarkers to confirm
bacterial infection are not always reliable or available, evidence-based guidance tends to fall behind current clinical
practice given the rapidly changing situation with AMR, and education and support for clinicians and patients may be lacking.2
A strategy that may help to address some of these factors is to have a practice policy in place that offers guidance
on when to use, and when not to use topical antibiotics, and how to discuss this with patients. Knowing that the practice
offers a consistent approach may give prescribers more confidence in their decision-making.
How can prescribers manage patient expectations for an antibiotic?
Patients with skin infections usually expect treatment with antibiotics, even if their infection is minor. Patient education
is an important aspect in reducing the use of all antibiotics, both topical and oral.
Successful interventions to help clinicians prescribe antibiotics rationally include:15
- Clear communication that reinforces appropriate use of antibiotics and the increasing problem of resistance; topical
antiseptics are recommended first-line for minor skin infections and if an antibiotic is required, oral treatment
will be necessary
- Setting realistic expectations regarding the natural history of the skin infection and the likely time for resolution;
many minor skin infections are self-limiting, “a nuisance rather than a problem” to the patient, and when
this is the case, best practice is to not prescribe at all.8
- Individualised prescribing; consider factors such as the patient’s age, severity of the infection, co-morbidities,
family and household circumstances
- A delayed prescription for an oral antibiotic may be of value in some situations provided the patient knows when and
why to get the prescription dispensed
Many issues remain unresolved regarding the appropriate use of topical antibiotics, such as clear evidence of effectiveness
of other treatments including topical antiseptics. Experts are calling for informed debate and further research, and it
is hoped that this will help determine the best course of action. In New Zealand, a randomised controlled trial is currently
underway, comparing the effectiveness of hygiene measures, topical antiseptics and topical fusidic acid in the management
of children with impetigo.7
At this stage, we recommend following the pragmatic advice: use topical antiseptics, along with good skin hygiene,
to treat minor skin infections, and oral antibiotics for more severe or extensive infection. The clinical
evidence is not yet conclusive, but the problem of rapidly rising resistance cannot be ignored. Watch
this space.
-
1986 - 1991
Mupirocin was available in New Zealand as a prescription-only medicine6
-
1991 - 2000
Mupirocin was available to purchase over-the-counter in New Zealand and was widely used
-
2000 - 2009
Mupirocin reverted to a prescription-only medicine due to concern about increasing resistance rates, particularly
in methicillin-resistant
S. aureus (MRSA).6 This resulted in a significant decrease in the use of mupirocin and a corresponding
decrease in resistance to mupirocin in
S. aureus from 28% in 1999 to 11% in 2013.13 However, over the 2000s, fusidic acid dispensing
rose rapidly along with a significant increase in the prevalence of resistance to fusidic acid
in S. aureus.13
-
2009
A bpacnz article on management of
impetigo recommended topical fusidic acid as initial treatment for children with small localised patches of impetigo
-
2012
Nurse-led school clinics for the assessment and treatment of children with skin infections, e.g.
the Mana Kidz programme in Counties Manukau District Health board, recommended topical fusidic acid first-line.14
-
2014
bpacnz article “Topical antibiotics: very few indications for use”
- Highlighted the increasing prevalence of resistance to fusidic acid in S. aureus
- Concluded that there were very few indications for use of topical antibiotics for skin infections
- Recommended that topical antibiotics should be considered only for patients with small, localised patches of
impetigo and occasionally for those with small, localised patches of infected eczema
-
-
2017
The current situation:
- Good skin hygiene and the use of topical antiseptic preparations are considered satisfactory initial treatment
options in the management of most patients with skin infections. Topical antibiotics should rarely be used
- Infectious disease experts advise that topical antibiotics should no longer be prescribed
as a first-line option for the majority of children with impetigo;* a topical antiseptic can be used for localised areas of infection
- If antibiotics are required for skin infections including impetigo and infected eczema, oral antibiotics are recommended
*Guidance for the management of impetigo has been recently updated in the bpacnz
Antibiotic
Guide to reflect this change in practice. The Antibiotic Guide is currently under revision and due to be completed in 2017.





